Non-Contrast MRI: A Game-Changer for Peripheral Artery Disease Detection?
"Discover how non-contrast MRI angiography at 3T offers comparable accuracy to traditional methods for diagnosing lower extremity arterial disease, providing a safer alternative for patients with PAD."
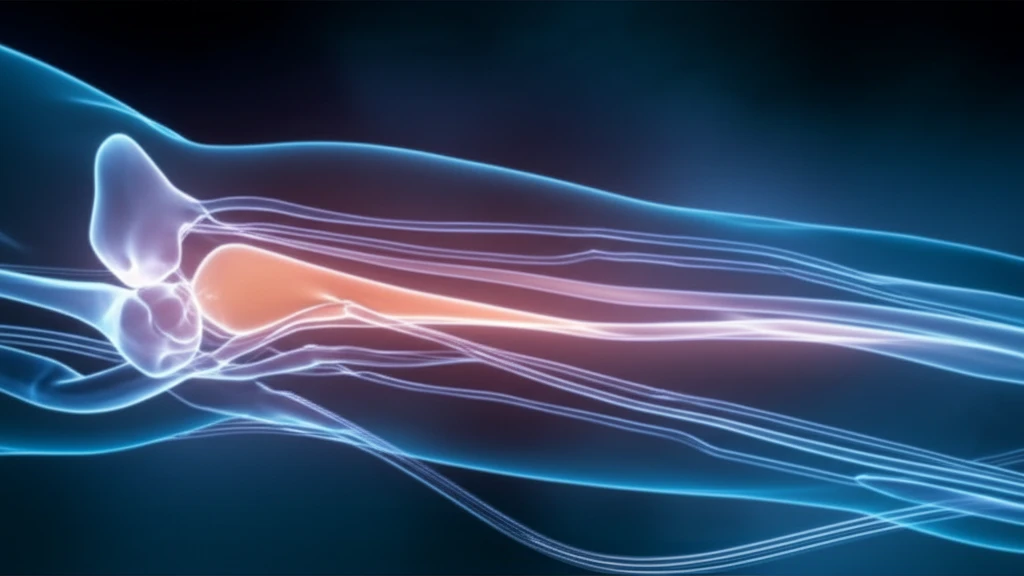
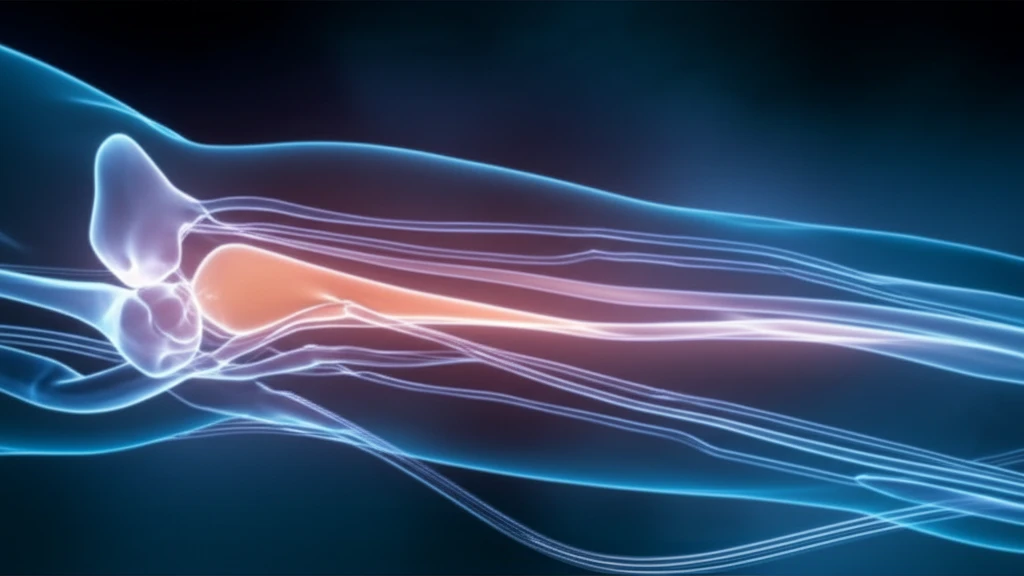
Peripheral artery disease (PAD) affects millions, often leading to significant mobility issues and pain. Traditionally, magnetic resonance angiography (MRI) with gadolinium-based contrast agents has been the go-to method for diagnosing PAD. However, concerns about nephrogenic systemic fibrosis and gadolinium accumulation in the brain have spurred the search for safer alternatives.
Enter non-contrast MRI angiography. Several techniques have emerged, aiming to provide accurate diagnostics without the risks associated with gadolinium. These methods capitalize on the natural properties of blood flow and advanced imaging technologies to visualize the arteries in the lower extremities.
A recent study published in the Journal of Vascular and Interventional Radiology compared two established non-gadolinium MR angiography protocols—QISS and QIR/ECG-FSE—with traditional gadolinium-enhanced MR angiography at 3T. The goal was to assess their diagnostic accuracy in detecting and characterizing lower extremity peripheral arterial disease. Here’s what they found.
Non-Contrast MRI Angiography: How Does It Work?
Before diving into the study's findings, it's important to understand the two non-contrast MRI techniques evaluated:
- QISS (Quiescent-Interval Single-Shot): This technique uses balanced steady-state free precession readout, time-of-flight effects, and a tracking saturation band to capture images of inflowing arterial blood. It doesn't require image subtraction, making it less susceptible to motion artifacts.
- QIR/ECG-FSE (Quadruple Inversion Recovery/Electrocardiogram-Gated Fast Spin Echo): This method combines quadruple inversion recovery for the abdominopelvic region with ECG-gated fast spin echo for the extremities. ECG gating helps to reduce motion artifacts by timing the image acquisition with the cardiac cycle.
The Future of PAD Diagnosis: Non-Contrast MRI
The study's findings suggest that QISS and QIR/ECG-FSE MR angiography protocols offer comparable diagnostic accuracy to gadolinium-enhanced MRI, particularly in terms of specificity. This means they are good at correctly identifying patients who do not have significant arterial disease. Either protocol could serve as a viable alternative for patients with PAD, especially those who cannot receive gadolinium-based contrast agents. As technology advances and imaging times are reduced, non-contrast MRI is likely to play an increasingly important role in the diagnosis and management of PAD.
