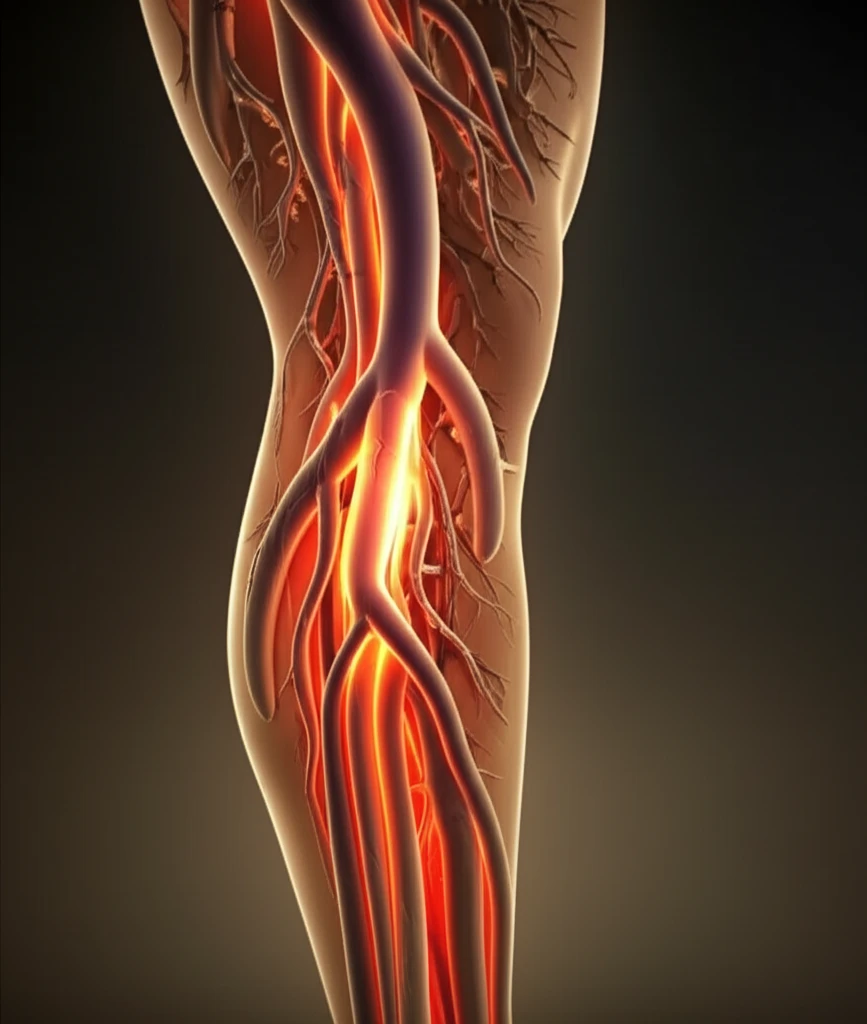
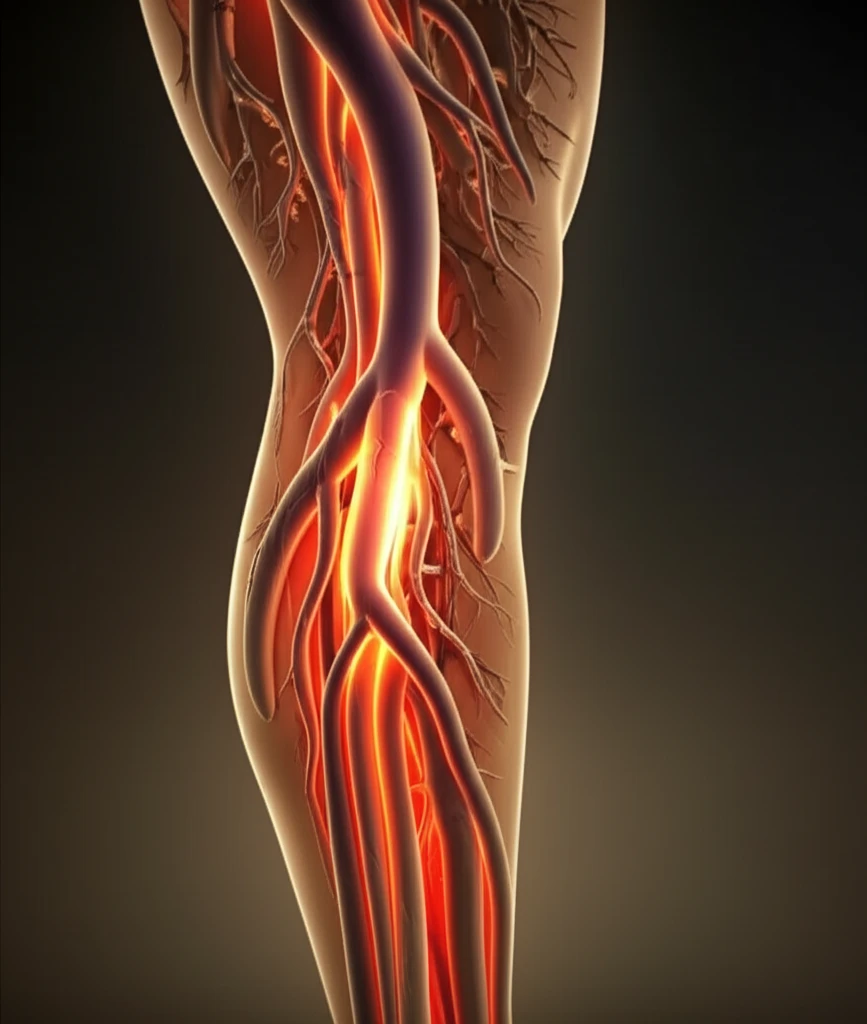
Bovine Carotid Artery Graft: A Promising Solution for Leg Bypass?
"Exploring the Long-Term Success of Artegraft in Lower Extremity Revascularization"
For years, biological grafts have played a vital role as vascular conduits in leg bypass surgeries. However, information specifically on bovine carotid artery grafts (BCAG) in lower extremity revascularization has been limited. This article explores the outcomes of lower leg bypass procedures using BCAG, offering insights into its effectiveness and long-term results.
This analysis is based on a retrospective review of a prospectively collected database, examining patients who underwent lower extremity bypass using BCAG from 2002 to 2017. The study focused on clinical outcomes, including graft patency (how long the graft stays open and functional) and limb salvage rates.
A total of 124 BCAG (Artegraft, North Brunswick, NJ) were implanted in 120 patients for lower extremity revascularization. The surgical indications varied, including disabling claudication (12%), rest pain (36%), tissue loss (48%), and infected prosthetic graft replacement (3%). In a significant number of cases (72%), the patient's own saphenous vein was either inadequate or absent, making BCAG a crucial alternative.
Why Choose BCAG for Lower Extremity Bypass?
BCAG was used in 46 patients (37%) who had a prior failed ipsilateral leg bypass. The distal anastomosis, where the graft connects to the artery, was performed in different locations: above-knee popliteal artery (25%), below-knee popliteal artery (26%), and tibial artery (39%). Notably, a distal anastomotic patch was created in all tibial artery cases to allow for BCAG-tibial reconstruction.
- Compliant.
- Thromboresistant.
- Durable.
- Easy to handle with surgical manipulation and suturing.
The Future of BCAG in Vascular Surgery
BCAG emerges as a reliable vascular conduit, offering good long-term results in lower extremity bypass procedures. This is particularly significant for patients lacking suitable autologous vein grafts.
BCAG offers several advantages. Biological grafts are associated with a lower risk of infection and enhanced graft anastomotic compliance due to their vessel elasticity, while BCAG's structural elasticity and ease of handling during suturing contribute to its appeal among surgeons.
While this study provides valuable insights, further prospective research is needed to compare BCAG with autogenous vein grafts directly. This will help refine our understanding of BCAG's role in lower extremity revascularization and optimize patient outcomes.
