Smarter Antibiotics: How Nanoparticles and Targeted Delivery Could Beat Pneumonia
"Could nanotechnology solve antibiotic resistance? New research explores how nanoparticle delivery can dramatically improve antibiotic effectiveness against severe infections like tularemia."
Pneumonia remains a major global health threat, and the rise of antibiotic-resistant bacteria is making treatment increasingly difficult. Traditional antibiotics often require high doses, leading to side effects and contributing to resistance. Scientists are now exploring innovative drug delivery systems to combat these challenges, with nanotechnology showing particular promise.
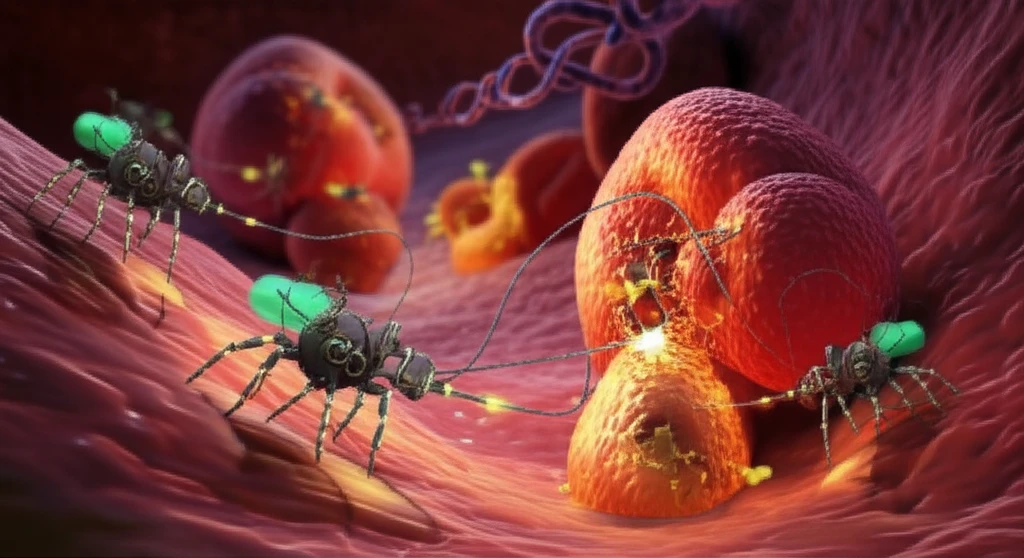
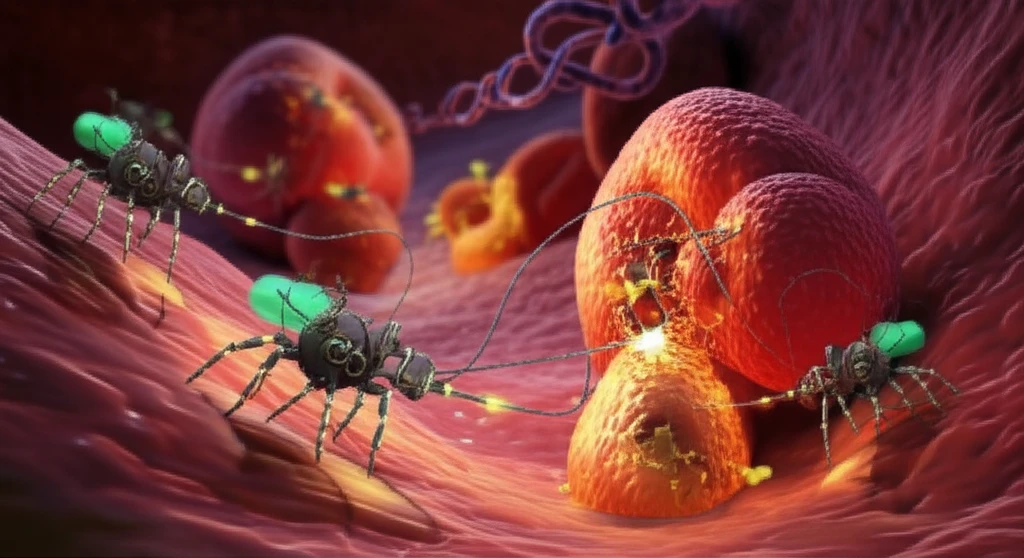
One such approach involves using nanoparticles – tiny particles designed to carry drugs directly to the site of infection. These nanoparticles can be engineered to release their payload in response to specific triggers, maximizing the drug's impact while minimizing its exposure to healthy tissues. This targeted delivery could revolutionize how we treat severe infections, improving outcomes and reducing the spread of resistance.
Recent research has focused on using mesoporous silica nanoparticles (MSNs) to deliver moxifloxacin, a powerful antibiotic, against pneumonic tularemia, a rare but serious infectious disease. This research is not just about tularemia; it offers valuable insights into how nanoparticle delivery can overcome limitations of traditional antibiotics for a range of infections.
Nanoparticle Delivery: A More Effective Approach
A study published in ACS Infectious Diseases investigated the effectiveness of moxifloxacin-loaded MSNs in treating pneumonic tularemia in mice. The researchers compared different routes of administration (intravenous, intramuscular, and subcutaneous) for both free moxifloxacin and MSN-encapsulated moxifloxacin. The results were striking: MSN-encapsulated moxifloxacin delivered intramuscularly (i.m.) was significantly more effective than free moxifloxacin, regardless of the route of administration.
- Prolonged Drug Release: The nanoparticle encapsulation extended the half-life of moxifloxacin, meaning the drug remained in the bloodstream longer.
- Sustained Therapeutic Levels: Intramuscular administration of MSN-moxifloxacin resulted in the longest time above the minimum inhibitory concentration (t>MIC), which is the concentration needed to stop bacterial growth.
- Targeted Action: Improved antibiotic delivery can act against F. tularensis at infection sites.
The Future of Antibiotics: Smarter, Not Just Stronger
This research highlights the potential of nanotechnology to transform antibiotic therapy. By focusing on optimizing drug delivery rather than simply increasing drug potency, scientists can:
<ul><li>Overcome resistance mechanisms</li><li>Reduce side effects</li><li>Improve treatment outcomes for severe infections.</li></ul>
While further research is needed to translate these findings into clinical applications, the study provides a compelling case for exploring nanoparticle-based drug delivery as a key strategy in the fight against antibiotic resistance. The integration of more targeting approaches can facilitate better outcomes for i.v. route of administrations.
