Shoulder Pain After Surgery? Unveiling the Truth About Rotator Cuff Repair Techniques
"Discover the latest research on arthroscopic rotator cuff repair and how different methods affect your recovery and long-term shoulder health."
Shoulder pain can be debilitating, significantly impacting your quality of life. For those suffering from rotator cuff tears, arthroscopic rotator cuff repair (ARCR) offers a promising solution. But with various surgical techniques available, understanding which approach is best is essential for a successful outcome. This article breaks down a recent study comparing two popular methods: suture bridge techniques with and without medial knot tying. We'll explore the findings and discuss how these techniques influence your recovery and long-term shoulder health.
ARCR is a minimally invasive procedure that aims to repair the torn tendons of the rotator cuff, a group of muscles and tendons that surround the shoulder joint. While the surgery itself is crucial, the specific technique used can have a significant impact on healing, pain levels, and overall function. The choice of technique can affect factors like initial fixation strength and the potential for re-tears, making it a key consideration for both surgeons and patients.
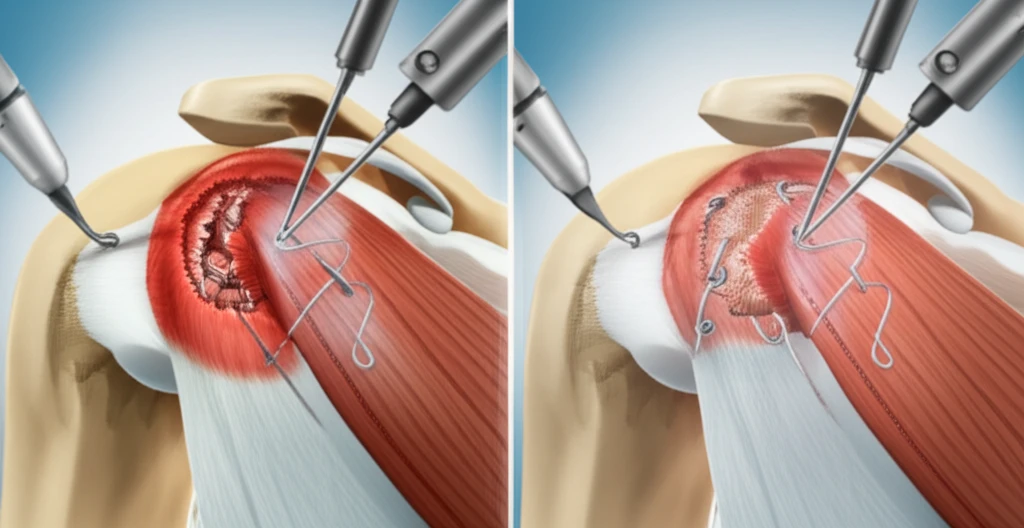
This article examines the outcomes of patients who underwent ARCR using different suture bridge techniques. Suture bridge techniques are designed to provide robust initial fixation. However, the addition of medial knot tying, while intended to enhance the repair, has raised questions. By comparing these two approaches, we aim to provide clarity on which method may offer the best chance for a full recovery and a return to pain-free shoulder function.
Suture Bridge Techniques: A Closer Look
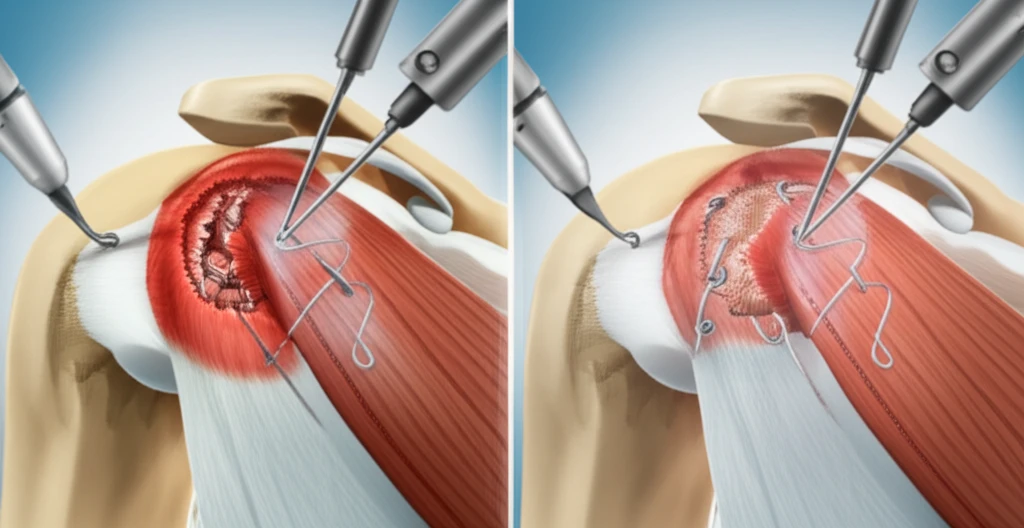
The study focused on two variations of the suture bridge technique, both commonly used in ARCR. These methods involve using sutures to bridge the torn tendon back to the bone. The critical difference lies in the presence or absence of medial knot tying. In the technique with medial knot tying, surgeons tie knots in a medial row, theoretically enhancing the repair's biomechanical strength. The technique without medial knot tying, on the other hand, relies on the suture bridge alone for fixation.
- Clinical Outcomes: Both WMT and WOMT groups showed significant improvements in JOA and UCLA scores over time, indicating improvements in function and pain reduction. There were no significant differences between the two groups in terms of these clinical outcomes.
- Re-tear Rates: The study found no significant difference in the rates of re-tears (Sugaya types 4 and 5) between the two groups at any of the follow-up points (3, 12, and 24 months).
- Healing: While complete healing (Sugaya type 1) rates were similar between the groups at 3 and 12 months, the WOMT group showed significantly better complete healing at 24 months. Conversely, the WMT group had a significantly higher number of incomplete healing cases (Sugaya types 2 and 3) at 24 months.
Key Takeaways and Implications for Patients
This research provides valuable insights for both patients and surgeons. It emphasizes the importance of considering the long-term structural outcomes when choosing a surgical technique. For patients, this means having an informed discussion with your surgeon about the potential benefits and drawbacks of each approach. While both techniques can provide pain relief and improved function, the study suggests that the technique without medial knot tying may offer a better chance for complete healing and long-term durability. As always, individual results may vary, and the best approach depends on various factors, including the size and type of tear, patient age, and activity level. Consulting with your surgeon to determine the most appropriate treatment plan for your specific needs is always recommended.
