Navigating Cervical Spine Surgery: A Patient-Centric Guide to Lateral Mass Fixation
"Demystifying surgical techniques for cervical spine stabilization, empowering patients with knowledge about lateral mass screws and optimized recovery."
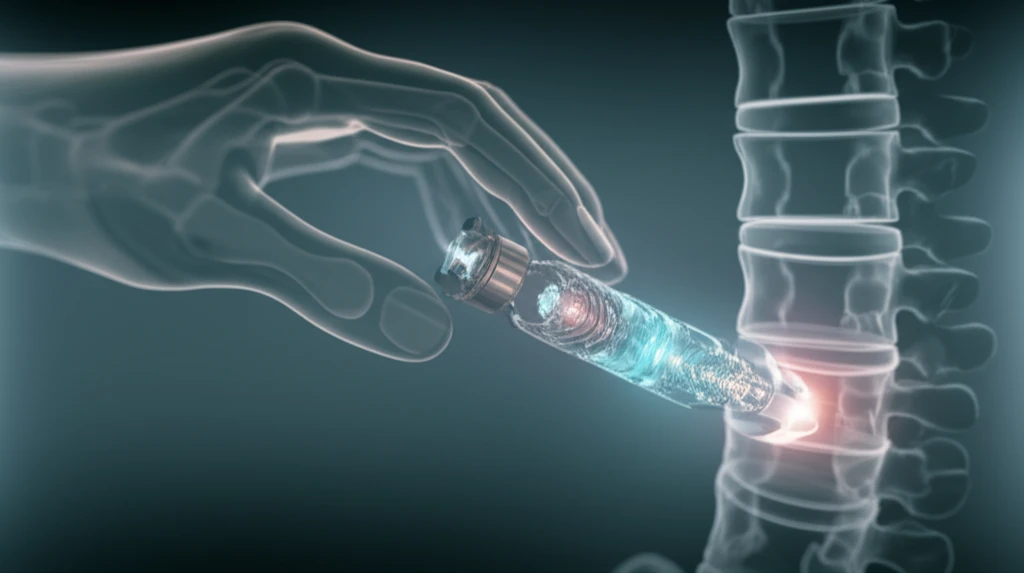
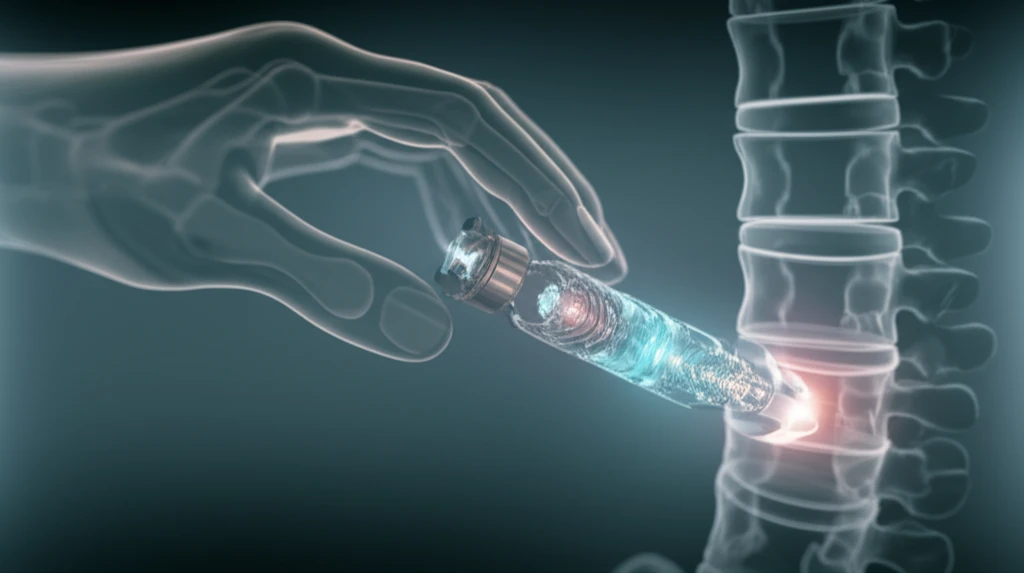
Cervical spine surgery can be a daunting prospect, filled with complex terminology and intricate procedures. One common technique used to stabilize the cervical spine, particularly in the subaxial region (C3-C7), involves the placement of lateral mass screws. This guide aims to demystify this procedure, providing patients and their families with a clearer understanding of what to expect.
Lateral mass fixation is often employed when there's instability in the cervical spine due to trauma, degenerative conditions, or other factors. The goal is to provide immediate stability and promote long-term fusion of the affected vertebrae. While the core principles of lateral mass fixation remain constant, surgical techniques continue to evolve, seeking to enhance precision and minimize complications.
This article synthesizes insights from a surgeon's perspective on optimizing the placement of lateral mass screws, focusing on a technique refined through years of experience. By understanding the nuances of this approach, patients can engage in more informed discussions with their surgeons and better prepare for the journey toward spinal health.
Understanding the Surgeon's Perspective on Lateral Mass Screw Placement
Lateral mass screw placement isn't just about following a textbook; it requires a deep understanding of individual patient anatomy and potential distortions caused by osteophytes or previous injuries. Standard measurements and angles may not always be applicable in real-world scenarios.
- Dissection and Identification: The surgeon carefully exposes the posterior lateral mass, identifying key landmarks like the valley between the lamina and the ridge of the lateral mass.
- Trajectory Planning: With a clear view, the surgeon mentally constructs a “slanted cube,” defining the longest possible trajectory for the screw, running diagonally from bottom medial to top lateral.
- Entry Point Considerations: Special attention is paid to the facet joint to maintain a safety margin.
- Alignment and Adjustment: The surgeon uses a Penfield instrument to target the ventral zone of the lateral mass, sometimes needing to adjust for anatomical variations by trimming the posterior spinous processes.
- Drilling Technique: High-speed power drills are used to create the initial entry point, followed by a powered device at low speed to advance the drill bit. Finger pressure controls ensure precision.
- Bicortical Purchase: The goal is to achieve bicortical purchase, meaning the screw passes through both layers of the bone, providing optimal stability. A long drill bit allows for flexible bending if bony prominences are encountered.
Long-Term Outcomes and Considerations
The benefits of this technique include using standard-sized screws, typically ranging from 14 to 20 mm, which are suitable for most adult patients. Surgeons also perform a pullout test to ensure each screw's stability. The exit point of the drill bit is carefully placed to avoid injury to the vertebral artery. Furthermore, the technique allows for a wide area to be prepared for grafting, promoting fusion.
