Lumbar Disc Microsurgery: Is It Still a Relevant Option for Back Pain Relief?
"Exploring the enduring role of lumbar disc microsurgery in modern back pain management and rehabilitation."
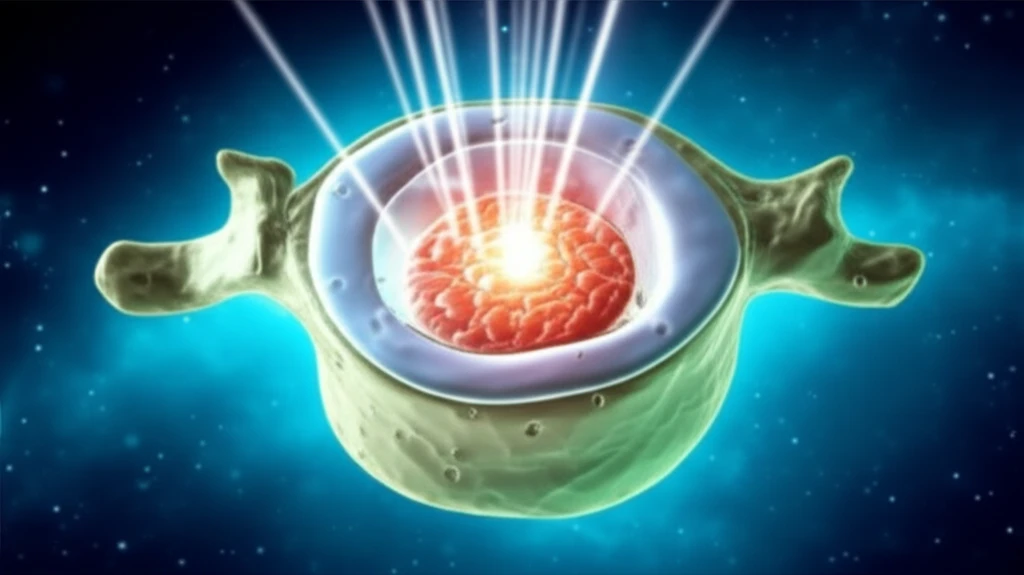
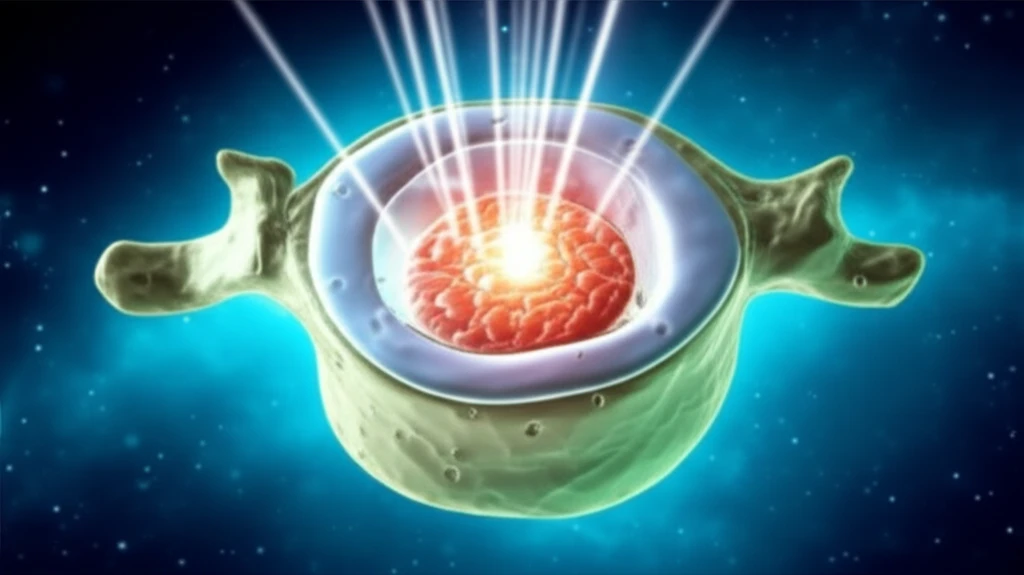
In 1953, the introduction of the surgical microscope by Zeiss marked a turning point in surgical procedures. The enhanced magnification and illumination capabilities allowed surgeons to operate with greater precision and minimal invasiveness. This innovation shifted the focus toward reducing tissue disruption while achieving surgical goals, establishing a new standard in surgical care.
The advent of microsurgery enabled surgeons to refine their techniques, fostering a deeper understanding of tissue behavior under stress. By minimizing manipulation of sensitive tissues, surgeons observed improved patient outcomes and quicker recovery times. This shift highlighted the importance of preserving normal anatomy during surgery, ultimately enhancing the body's natural healing processes.
Moreover, microsurgery emphasized the critical link between surgical precision and rehabilitation. Surgeons recognized that the initial surgical intervention plays a crucial role in the overall rehabilitation process. This understanding transformed the approach to patient care, integrating surgery as the first step toward recovery rather than a separate, later stage intervention.
When Is Lumbar Disc Microsurgery the Right Choice?
Lumbar microsurgery is primarily indicated for patients suffering from herniated lumbar discs and, in certain instances, spinal stenosis. The decision to proceed with microsurgery is typically based on the presence of specific symptoms associated with disc herniation, including:
- Severe and persistent leg pain
- Numbness in the legs
- Muscle weakness in the legs
- Bowel or bladder dysfunction
Author's Insights: Optimizing Outcomes in Lumbar Disc Microsurgery
The success of lumbar microsurgery hinges on several factors, including the duration of spinal nerve compression and the underlying biology of the disc herniation. The available space for the spinal nerve and the extent of compression significantly influence outcomes. Surgery is most effective when performed within three months of nerve compression. The degree of herniation observed during surgery correlates with results more accurately than MRI scans. Large disc herniations often yield better outcomes than marginal protrusions, although exceptions exist. Even small protrusions can cause significant pressure in conjunction with spinal stenosis.
