Dialysis Dilemma: Which Type Offers Better Survival with Artery Disease?
"A 6-year study reveals surprising survival differences between hemodialysis and peritoneal dialysis patients with subclinical peripheral artery disease."
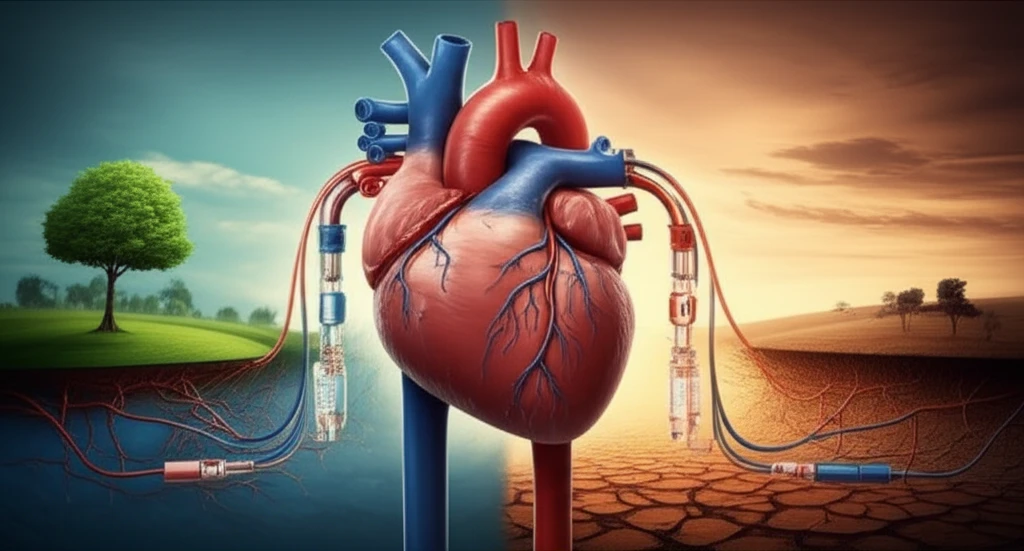
For individuals grappling with end-stage renal disease (ESRD), the road is fraught with challenges, especially when cardiovascular complications enter the picture. Peripheral artery disease (PAD), a condition affecting blood flow to the limbs, is a frequent and dangerous co-conspirator in ESRD, significantly raising the risk of mortality. Choosing the right treatment approach becomes paramount, and the two main options, hemodialysis (HD) and peritoneal dialysis (PD), have been a topic of intense debate among medical professionals.
Both hemodialysis and peritoneal dialysis serve as critical renal replacement therapies, but questions linger about their comparative effectiveness, particularly for high-risk groups. While some studies suggest they're equivalent, others point to conflicting outcomes, especially when considering pre-existing conditions like cardiovascular disease. This raises a crucial question: Can one dialysis modality offer a survival advantage for ESRD patients also battling PAD?
A recent study, published in the International Journal of Medical Sciences, sought to answer this very question. Researchers compared survival rates between HD and PD patients who also had subclinical PAD, defined as an ankle-brachial index (ABI) of less than 0.9. The findings revealed some unexpected differences, offering new insights into optimizing treatment strategies for this vulnerable population. This article breaks down the study's methodology, results, and what they mean for patients and healthcare providers alike.
HD vs. PD: Unpacking the Survival Rates
The research team followed 91 patients with both ESRD and subclinical PAD over six years, carefully tracking their outcomes and causes of mortality. What they discovered challenges some common assumptions about dialysis treatment. The study revealed that patients undergoing peritoneal dialysis (PD) had a statistically significant higher mortality rate compared to those undergoing hemodialysis (HD).
- Higher Cardiovascular Mortality in HD: Interestingly, the study found that HD patients experienced a higher rate of cardiovascular-related deaths compared to the PD group.
- Increased Risk of Infection in PD: Conversely, PD patients had a greater percentage of deaths due to infection.
- Impact of Residual Renal Function: The study also explored the role of residual renal function (the kidney's ability to still function) in PD patients. Those with no residual renal function (anuric) appeared to have worse survival outcomes.
Making Informed Decisions: What This Means for Patients and Doctors
The study's findings underscore the importance of individualized treatment plans for ESRD patients with PAD. While HD may offer a survival advantage in this specific scenario, the choice of dialysis modality should always be a collaborative decision between the patient and their nephrologist, considering the patient's overall health status, lifestyle, and preferences.
Moreover, this research emphasizes the need for careful monitoring and management of cardiovascular risk factors in all ESRD patients, regardless of dialysis type. Vigilant attention to blood pressure, cholesterol levels, and other risk factors can help mitigate the dangers of PAD and improve overall outcomes.
While this study provides valuable insights, it also calls for further research. Larger, prospective studies are needed to confirm these findings and to investigate the underlying mechanisms driving the observed differences in survival rates. Understanding these mechanisms could pave the way for more targeted and effective interventions to improve the lives of ESRD patients with PAD. Furthermore, additional studies can reveal the importance of residual function and its correlation with PAD, especially for PD patients.
