Decoding Prostate Biopsy Results: Why Location Matters
"Understanding Discordance in Positive Cores for Better Prostate Cancer Management"
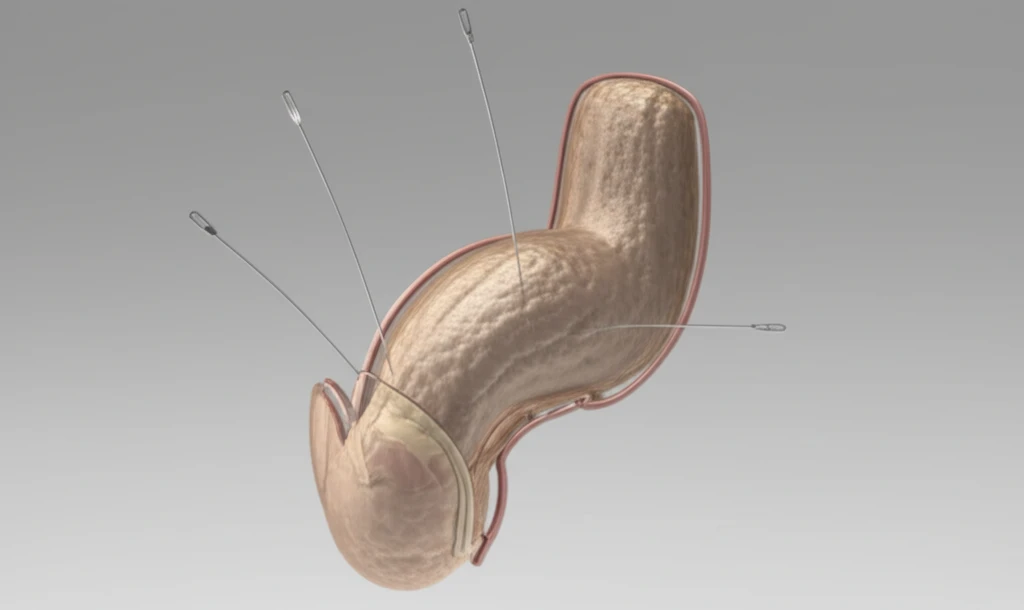
Prostate cancer is a leading health concern for men worldwide, ranking as the second most common cancer in males. Early and accurate detection is critical, and transrectal ultrasonography (TRUS) guided prostate biopsy has become a standard diagnostic tool. This procedure not only confirms the presence of cancer but also provides essential information about its location and extent.
The detailed information gleaned from a prostate biopsy plays a pivotal role in determining the most appropriate treatment strategy. Factors such as active surveillance, radical prostatectomy, and hormone therapy are all considered based on the biopsy's findings. During a radical prostatectomy, surgeons rely on biopsy data to decide how closely or widely to dissect, and whether to attempt to preserve the neurovascular bundle, which is vital for maintaining erectile function and continence.
However, TRUS-Bx isn't foolproof. Sampling limitations can lead to inaccuracies, with some cancers going undetected. This is particularly concerning when surgeons aim to preserve the neurovascular bundle, as undetected cancer in these areas can result in positive surgical margins (PSM), indicating that cancer cells remain after surgery. Recent research has focused on comparing the location of positive cores in biopsies with the location of PSMs to improve surgical outcomes.
Positive Surgical Margins and Discordance: Unpacking the Data
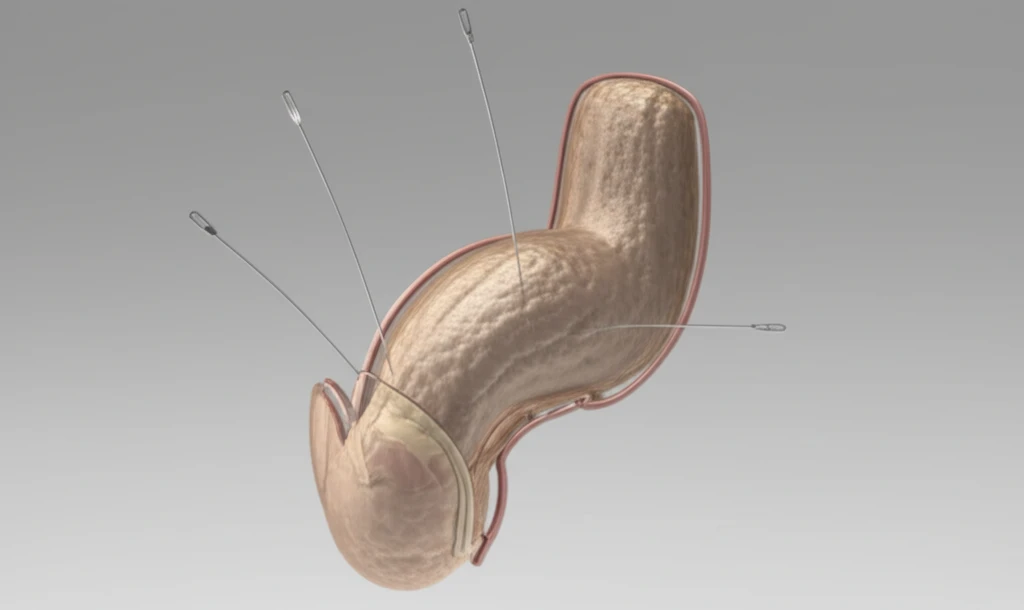
A recent study investigated the correlation between positive cores found during a prostate biopsy and the location of positive surgical margins (PSM) following radical prostatectomy. The study retrospectively analyzed data from patients diagnosed with prostate cancer via standard 12-core TRUS-Bx who subsequently underwent radical prostatectomy and were found to have PSMs. After excluding cases with fewer than 12 biopsy cores or incomplete location data, 46 patients with PSMs were included in the analysis.
- Most Common PSM Locations: The most frequent sites for PSMs were the right apex (n=21) and left apex (n=15).
- Multiple PSMs: Multiple PSMs were reported in 21 specimens (45.7%).
- Concordance vs. Discordance: In 32 specimens (69.6%), one or more concordant positive biopsy cores were identified. However, 14 specimens (28%) showed no concordant biopsy cores at the PSM location.
- Discordance Rate: When analyzed by location, the right apex PSM had the highest rate of discordance (38%).
- Patient Characteristics: The discordant group had significantly lower prostate volume and a lower number of positive cores in the biopsy compared to the concordant group.
Key Takeaways for Patients and Future Directions
This study emphasizes that a notable fraction of PSMs occur in areas where tumors were not initially detected by biopsy, with the apex region showing the highest discordance. This highlights the need for surgeons to exercise caution during dissection, especially in the apex, even when biopsy results are negative. Further research is needed to refine biopsy techniques, enhance imaging modalities, and develop more precise surgical strategies to minimize the risk of PSMs and improve outcomes for men undergoing radical prostatectomy for prostate cancer.
