Bone Regeneration Breakthrough: How Surface Texture and Materials Impact Healing
"Discover how altering spacer materials and micro-topography can enhance bone regeneration in the Masquelet technique."
The Masquelet technique represents a significant advancement in reconstructive bone surgery, particularly for addressing substantial bone defects resulting from trauma, tumor resection, or osteomyelitis. This innovative two-stage procedure harnesses the body’s natural healing capabilities by first creating a vascularized foreign-body membrane, which acts as a nurturing environment for subsequent bone graft incorporation.
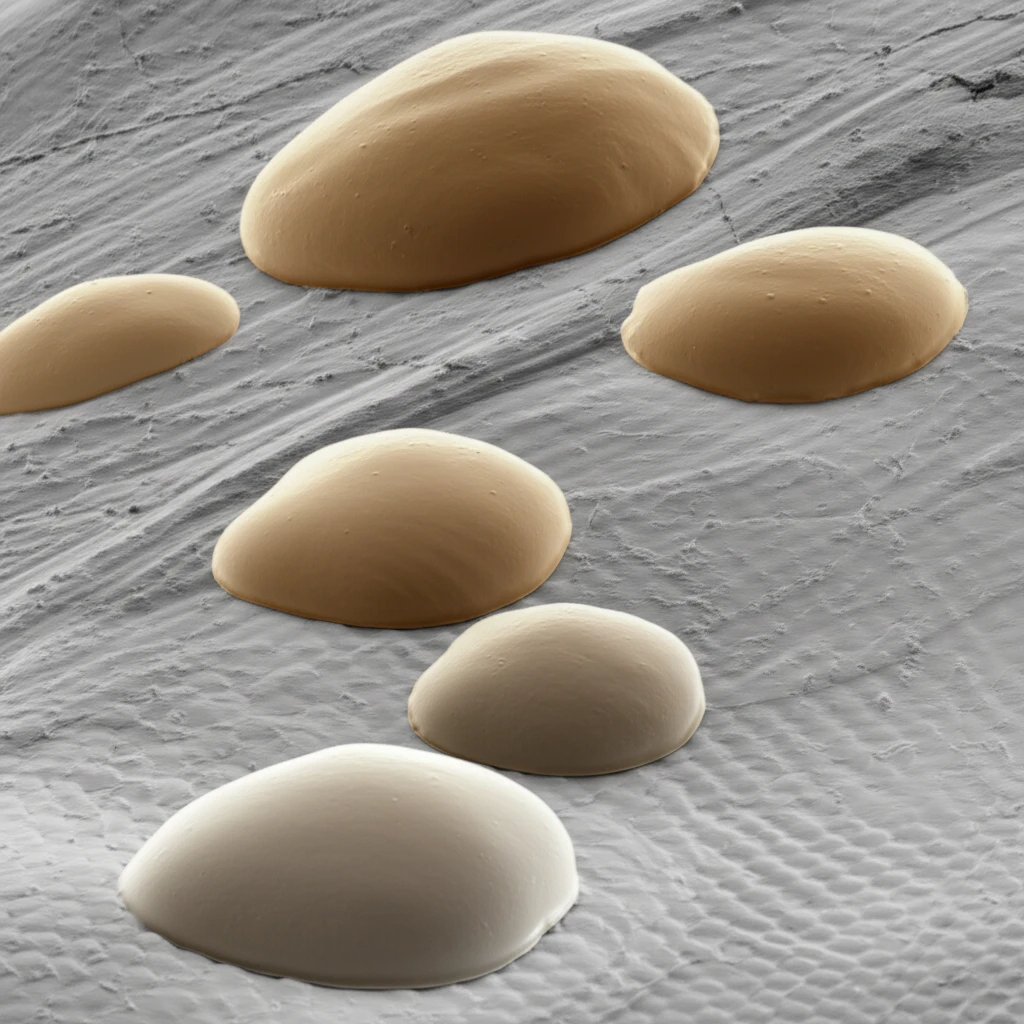
During the initial stage, a spacer—typically made of polymethyl methacrylate (PMMA), also known as bone cement—is implanted to stimulate membrane formation. This membrane serves not only as a physical barrier against soft tissue invasion but also as a reservoir of essential biochemical factors that promote bone regeneration. In the second stage, the spacer is removed, and the defect is filled with morselized bone graft, which then integrates within the protective and bioactive environment created by the membrane.
Recent studies have explored how modifying the surface characteristics of the implanted spacer can influence membrane development. These modifications, including variations in material composition and surface roughness, have shown promise in altering the mechanical and biochemical properties of the induced membrane. Understanding these effects is crucial for optimizing the Masquelet technique and enhancing bone regeneration outcomes.
Spacer Material and Surface Topography: Key Factors in Bone Regeneration
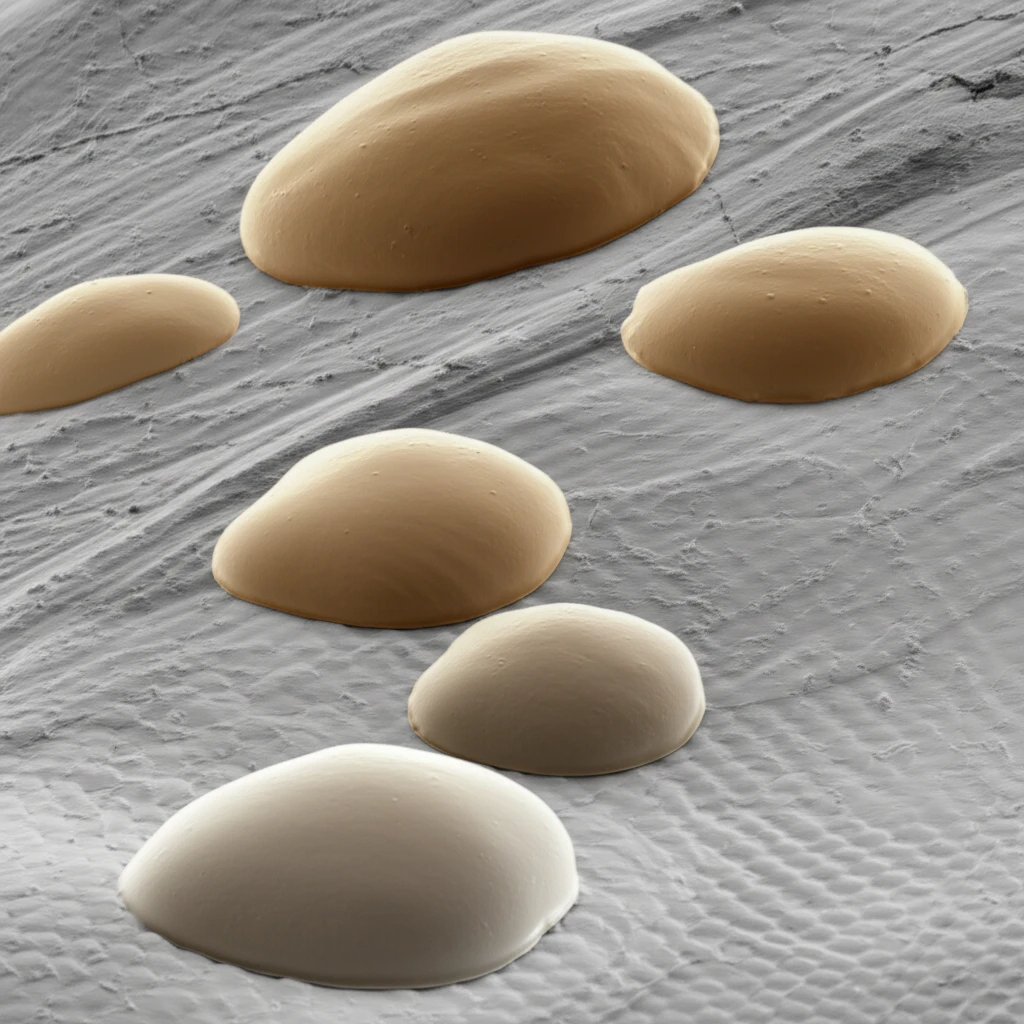
A recent study conducted by researchers at Saint Louis University School of Medicine delved into how different spacer materials and surface textures affect the biochemical environment of the induced membrane and, consequently, the process of bone regeneration. The study compared the effects of PMMA spacers with those made of titanium (TI), a material known for its biocompatibility and mechanical strength. Additionally, the spacers were prepared with either smooth or roughened surfaces to investigate the impact of micro-topography on membrane development and bone healing.
- PMMA (Polymethyl Methacrylate): Traditional spacer material, known as bone cement.
- TI (Titanium): Experimental spacer material, explored for its biocompatibility.
- TGFβ (Transforming Growth Factor Beta): Positive regenerative protein.
- BMP2 (Bone Morphogenetic Protein 2): Positive regenerative protein, promotes osteogenic differentiation.
- VEGF (Vascular Endothelial Growth Factor): Positive regenerative protein, promotes angiogenesis.
Implications for the Future of Bone Reconstruction
This research underscores that the induced membrane’s role in the Masquelet technique extends beyond mere physical support. Its biochemical environment plays a crucial part in orchestrating bone regeneration. Further studies are needed to fully elucidate the interplay between different spacer materials, surface textures, and the resulting cellular and molecular events within the membrane. By gaining a deeper understanding of these factors, clinicians can optimize the Masquelet technique to achieve more predictable and successful outcomes in bone reconstruction.
