Wound Debridement: A Comprehensive Guide to Methods and Best Practices
"Discover the essential techniques for effective wound debridement, ensuring optimal healing and reduced infection risk. Learn from real-world case studies."
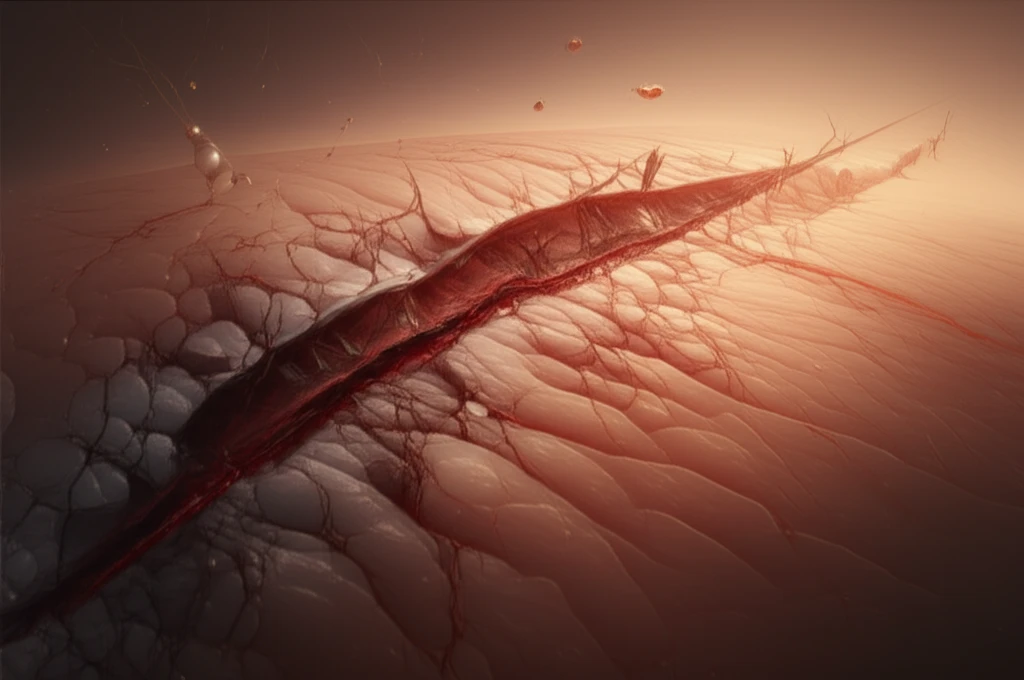
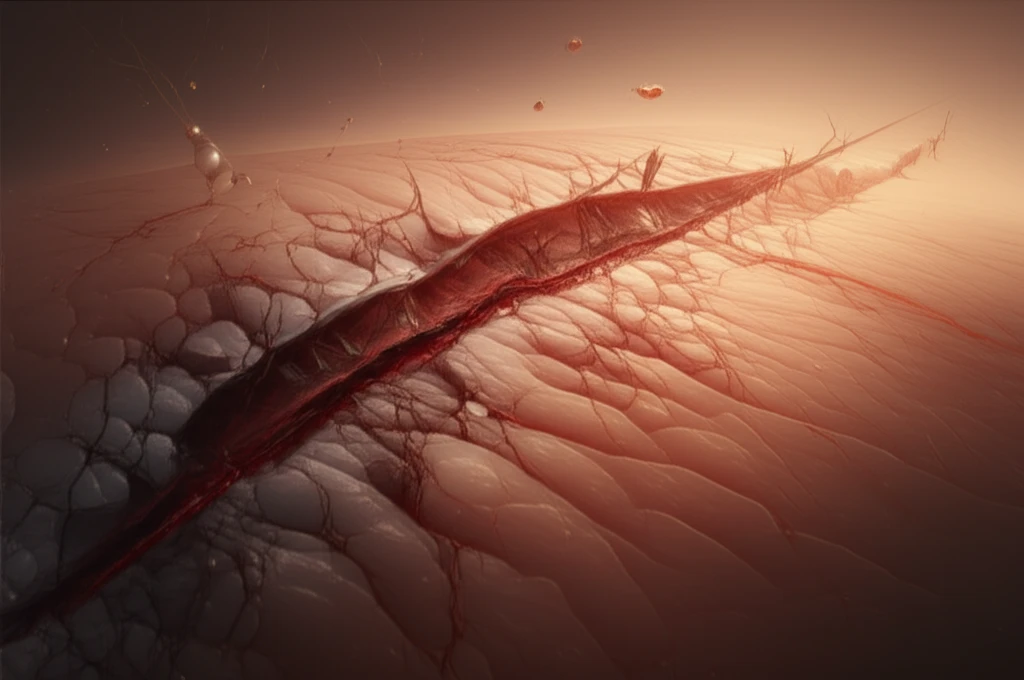
Wound debridement is a critical component of wound bed preparation, focused on removing foreign material, dead or damaged tissue, and debris from wounds. This process accelerates healing and reduces the risk of infection, leading to better patient outcomes.
Effective wound bed preparation, as highlighted by Fletcher (2005), involves creating an optimal healing environment. This includes managing wound exudate, restoring bacterial balance, and, most importantly, removing necrotic tissue (Dowsett 2002).
While high-quality evidence definitively proving the necessity of debridement is limited, existing research indicates that it significantly accelerates the healing process (NICE 2001, Falanga 2004, Gethin 2009) and reduces the risk of infection and sepsis (Leaper 2002).
Debridement Techniques: Choosing the Right Approach
Numerous techniques are available for wound debridement, each with unique advantages and disadvantages. These include autolytic, enzymatic, larval, mechanical, and surgical methods. Sharp debridement is often considered the 'gold standard' (Leaper 2002), but the optimal choice depends on the patient's specific needs and the wound's condition.
- Autolytic Debridement: Uses the body's own enzymes to break down dead tissue, often facilitated by hydrocolloid dressings.
- Enzymatic Debridement: Involves applying topical enzymes to dissolve necrotic tissue.
- Larval Debridement: Uses medical-grade maggots to consume dead tissue and stimulate healing.
- Mechanical Debridement: Physically removes dead tissue through methods like wet-to-dry dressings or irrigation.
- Surgical Debridement: The removal of dead tissue with scalpel and scissors.
Conclusion: Prioritizing Patient-Centered Wound Care
This article highlights the importance of a comprehensive approach to wound debridement, tailored to the individual needs of each patient. Effective debridement requires a thorough understanding of available techniques, careful assessment of the wound, and ongoing evaluation of treatment outcomes. With proper management, even complex wounds can progress toward healing, improving the patient's quality of life.
