When Chest Tubes Go Wrong: How a Vascular Plug Can Save the Day
"A minimally invasive technique offers a solution when a chest tube accidentally enters the liver."
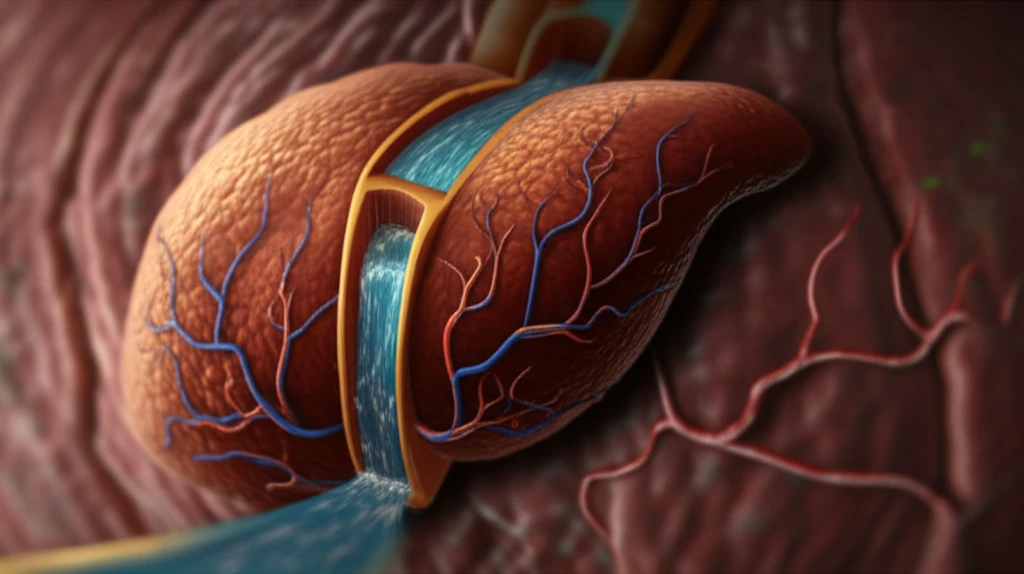
Chest tubes are essential tools in managing various thoracic conditions, such as pleural effusions and pneumothoraxes. However, the insertion of these tubes isn't always straightforward, and complications can arise, including misplacement. While rare, one particularly dangerous complication occurs when a chest tube inadvertently punctures the liver. This can lead to significant bleeding and require immediate intervention to prevent life-threatening consequences.
A recent case report highlighted in Cardiovascular and Interventional Radiology details a scenario where a 70-year-old man experienced this exact complication. Following chest tube insertion to address a collapsed lung and pleural effusion, the tube was found to have penetrated the liver, traveling through the hepatic vein and reaching the right ventricle of the heart. This prompted an emergency response and a clever solution from interventional radiologists.
Traditionally, managing such complications would involve more invasive surgical procedures. However, advancements in interventional radiology have paved the way for less invasive approaches. The article we're diving into showcases the use of an Amplatzer Vascular Plug (AVP) to effectively embolize, or block, the misplaced chest tube tract in the liver. This technique offers a minimally invasive alternative to open surgery, reducing patient risk and recovery time.
The Case of the Misplaced Chest Tube: A Step-by-Step Rescue
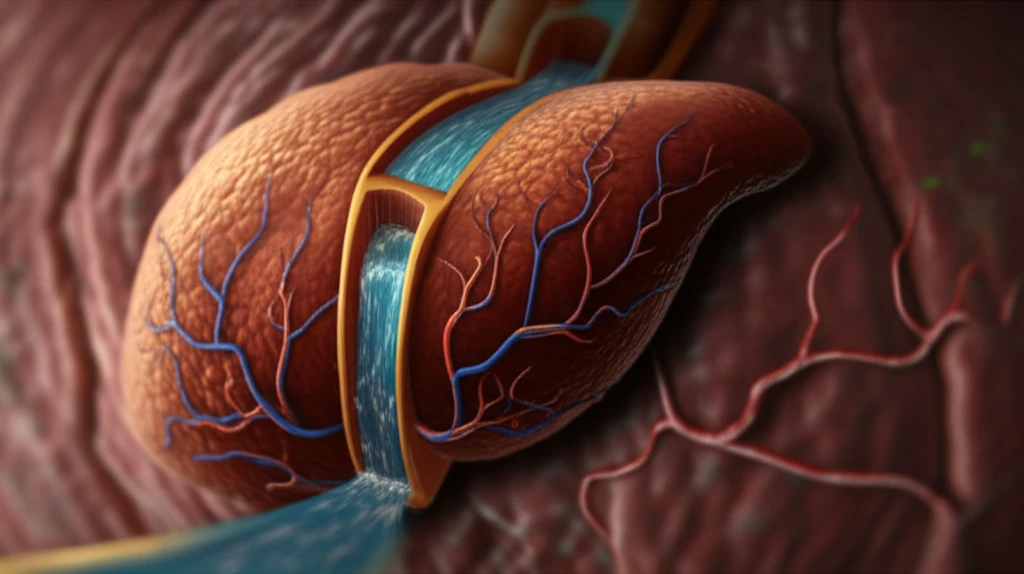
The initial chest tube insertion in the 70-year-old patient led to a rapid loss of blood, triggering cardiopulmonary resuscitation. Imaging revealed the alarming path of the chest tube through the liver and into the heart. Fortunately, the patient's condition was stabilized, allowing time for a planned intervention.
- Careful Withdrawal: Under fluoroscopic guidance, the chest tube was carefully withdrawn to the inferior vena cava (IVC), using the patient's vertebral contours as landmarks.
- Guidewire and Catheter Placement: A 0.035-inch hydrophilic guidewire and a 5-Fr catheter were advanced through the chest tube into the IVC, then pulled back into the hepatic vein, creating a pathway for the AVP.
- AVP Deployment: A 6-mm Amplatzer vascular plug (AVP) IV was advanced through the catheter and strategically placed to block the liver tract. The AVP was initially positioned in the hepatic vein and then pulled back to the hepatic parenchyma.
- Confirmation and Release: The team used a nearby liver calcification and patient feedback to estimate the vein-tract junction and ensure correct AVP placement. Once satisfied that there was no bleeding, the AVP was detached, and the chest tube and catheter were removed.
The AVP Advantage: A Safe and Effective Alternative
The use of AVPs to embolize errant chest tube tracts appears to be a safe and effective method, especially when compared to more invasive surgical options. The minimally invasive nature of the procedure translates to reduced patient risk, shorter recovery times, and a decreased likelihood of complications. However, it's important to note that patients with hepatic congestion may require alternative approaches, such as occlusive balloons, to manage bleeding effectively.
