When Antibodies Attack: Unraveling the Mystery of MPA and Cross-Reactions
"A rare case study reveals how microscopic polyangiitis can trigger antibodies that mimic Hantaan virus, shedding light on the complexities of autoimmune disorders."
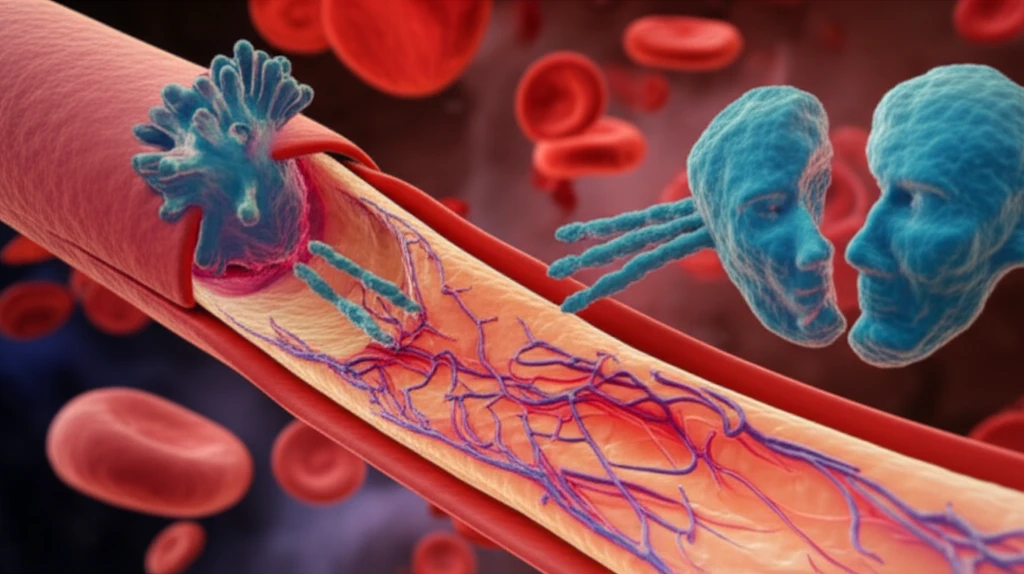
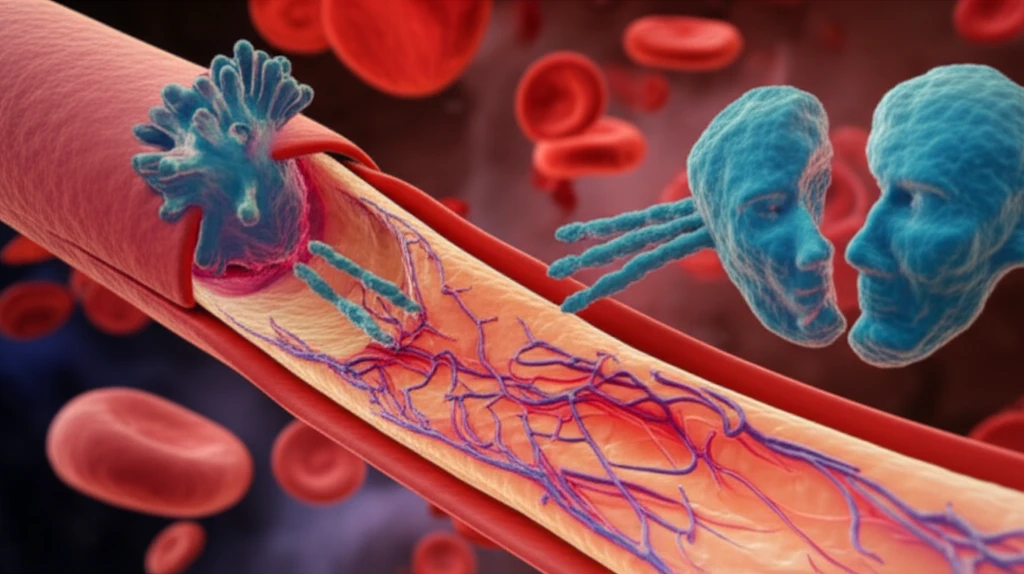
The human body's immune system is a marvel, designed to protect us from foreign invaders like viruses and bacteria. However, in some cases, this intricate defense system can go awry, leading to autoimmune disorders where the body attacks its own tissues. Microscopic polyangiitis (MPA) is one such condition, characterized by inflammation of small blood vessels. Patients with MPA often develop antineutrophil cytoplasmic antibodies (ANCAs), which target proteins within their own immune cells.
Hantaan virus, on the other hand, is a rodent-borne virus that can cause hemorrhagic fever with renal syndrome (HFRS), a severe illness affecting the kidneys and blood vessels. Diagnosis of HFRS relies on detecting virus-specific antibodies, particularly immunoglobulin M (IgM), in a patient's blood.
Now, imagine a scenario where a patient with MPA tests positive for Hantaan virus-specific IgM antibodies, even though they don't have HFRS. This seemingly paradoxical situation can occur due to a phenomenon called cross-reactivity, where antibodies generated against one target mistakenly recognize and bind to another, similar-looking target. A recent case study explores this intriguing interplay between MPA and Hantaan virus, highlighting the diagnostic challenges and potential mechanisms involved.
The Case: MPA Mimicking HFRS
The case study, published in Archives of Rheumatology, details the experience of a 71-year-old woman who was admitted to the hospital with fever, cough, and rapidly declining kidney function. Initial laboratory tests revealed elevated creatinine levels, indicating kidney damage. Further investigation revealed the presence of perinuclear ANCA and high levels of myeloperoxidase (MPO)-ANCA, both indicative of MPA. A kidney biopsy confirmed necrotizing crescentic glomerulonephritis, a hallmark of MPA affecting the kidney's filtering units.
- Antibody Specificity: Antibodies are highly specific, but not always perfect. They bind to target molecules (antigens) based on shape and chemical properties.
- Molecular Mimicry: Sometimes, different molecules share similar structural features. If an antibody developed against one molecule encounters a similar one, it might bind to it, even if it's not the intended target.
- Immune Disorders: Autoimmune diseases often involve a broader dysregulation of the immune system, increasing the likelihood of generating cross-reactive antibodies.
Implications and Future Directions
This case study underscores the importance of considering cross-reactivity in the diagnosis of MPA and other autoimmune disorders. While a positive test for Hantaan virus-specific IgM antibodies might initially suggest HFRS, clinicians should be aware that it could be a false positive due to cross-reactivity in patients with MPA. This is especially important for younger audience since the disease symptoms could be misleading to a more severe issue. Further research is needed to identify the specific antigens involved in this cross-reactivity and to develop more specific diagnostic tests. Understanding the mechanisms driving cross-reactivity could also lead to new therapeutic strategies for autoimmune diseases. For example, researchers are exploring ways to selectively eliminate or suppress the production of cross-reactive antibodies, while preserving the overall function of the immune system. Further studies will help doctors accurately diagnose and treat this rare condition and other similar autoimmune responses.
