Vasculitis and Kidney Biopsies: When Can You Skip the Procedure?
"Navigating the complexities of vasculitis diagnosis: A guide to understanding when a kidney biopsy is essential and when it might be safely avoided."
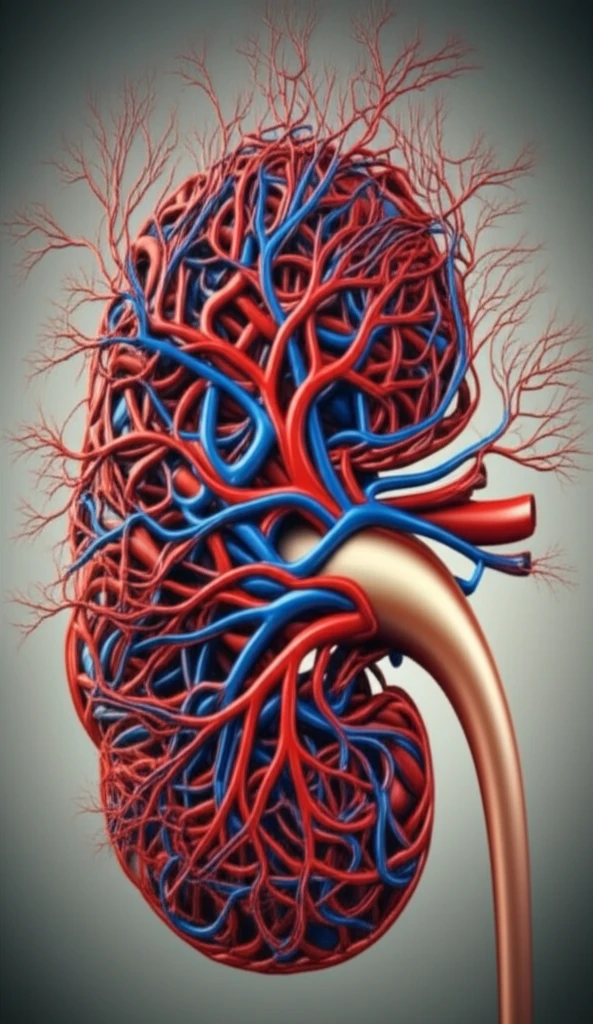
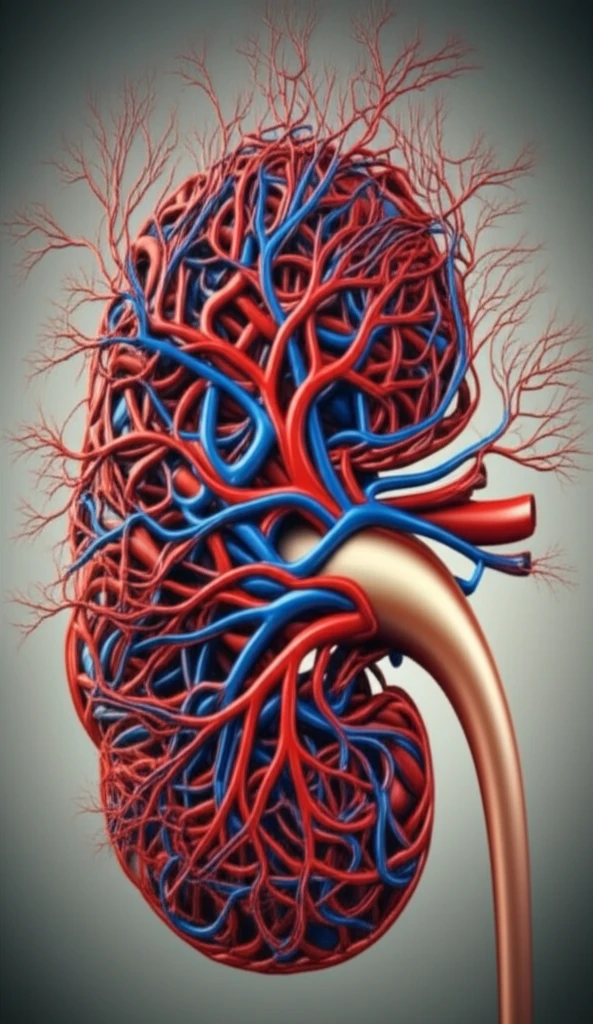
Vasculitis, a condition marked by inflammation of blood vessels, poses a significant threat to kidney health and can lead to end-stage renal disease (ESRD). Small-vessel vasculitis, in particular, stands out as a primary culprit behind rapidly progressive glomerulonephritis, a severe kidney ailment. Timely diagnosis and appropriate treatment are crucial to prevent irreversible damage and reduce the risk of ESRD and premature mortality.
The gold standard for diagnosing vasculitis has traditionally been renal biopsy, a procedure where a small piece of kidney tissue is extracted for examination. However, the advent of advanced serological testing, particularly assays for anti-neutrophil cytoplasmic antibodies (ANCA), has sparked debate about the necessity of biopsy in all cases of suspected ANCA-associated vasculitis (AAV).
This article delves into the complexities surrounding the decision to perform or forgo a kidney biopsy in suspected vasculitis cases. We'll explore the factors influencing this decision, weigh the reliability of serological tests, and discuss scenarios where biopsy might be safely avoided. This guide aims to empower patients and their families with the knowledge to navigate this challenging diagnostic landscape.
Can You Trust the Serology? Understanding ANCA Test Results
Serological testing, especially ANCA assays, plays a pivotal role in diagnosing vasculitis. Modern proteinase 3 (PR3) and myeloperoxidase (MPO)-ANCA assays have enhanced diagnostic accuracy, gradually replacing the less specific indirect immunofluorescence (IFF) test. These advanced assays, when combined with a patient's clinical presentation, form the cornerstone of informed decisions regarding biopsy.
- False Positives: ANCA tests can sometimes yield 'false positive' results, indicating vasculitis when none exists. Low-level positive or borderline values are often seen in conditions like hypergammaglobulinemia and myeloma.
- Assay Variability: Different ANCA assays may produce varying results, making it challenging to quantify ANCA levels accurately. A strong positive result in one assay might appear weak in another.
- ANCA-Negative Vasculitis: In a small percentage of pauci-immune crescentic nephritis cases (5-10%), ANCA is absent, despite the presence of AAV.
- Other Antibodies: Anti-GBM tests are generally reliable, but false positives and negatives can occur. ANA tests are often conducted concurrently, and MPO-ANCA can sometimes cause false-positive ANA results. Rheumatoid factor might be present in AAV patients, suggesting a secondary infection or cryoglobulinemia. Complement C3 levels are also increasingly scrutinized in AAV.
The Bottom Line: Informed Decisions for Better Outcomes
Deciding whether to perform a kidney biopsy in suspected vasculitis cases is a complex process that requires careful consideration of serological results, clinical presentation, and the expertise of the treating physician. While renal biopsy remains the definitive diagnostic tool, advancements in ANCA testing have opened the door to potentially avoiding biopsy in select cases. By understanding the nuances of serological testing and integrating these findings with clinical data, healthcare providers can make informed decisions that lead to better outcomes for patients with vasculitis.
