Unusual Blood Clots: When Vein Thrombosis Strikes in Unexpected Places
"Exploring rare venous thrombosis locations and what they reveal about underlying health conditions."
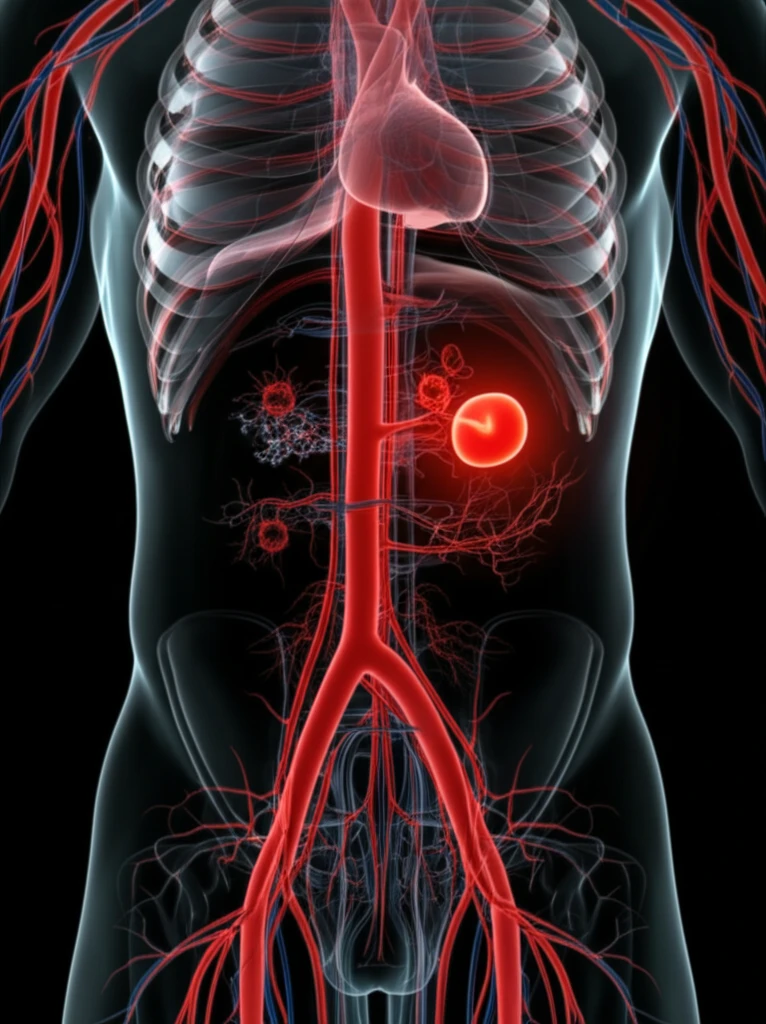
Deep vein thrombosis (DVT) is a serious condition where blood clots form in the veins, most commonly in the legs. However, DVT can also occur in less typical locations, such as the jugular, cerebral, or mesenteric veins. These unusual occurrences, known as venous thrombosis of an unusual site, prompt a more in-depth investigation to identify underlying causes.
Several studies presented at the 78th Congress of Internal Medicine in Grenoble shed light on the diagnostic and etiological aspects of these atypical thromboses. Understanding these rare cases is crucial because they often indicate underlying health issues that might otherwise go unnoticed. This is especially important for younger individuals, those without typical risk factors, or when thrombosis occurs in multiple sites.
This article synthesizes findings from these studies to provide a comprehensive overview of unusual venous thromboses, focusing on their clinical presentation, potential causes, and the role of diagnostic tools in uncovering these rare conditions.
Why Location Matters: Uncovering Clues from Atypical Thrombosis Sites
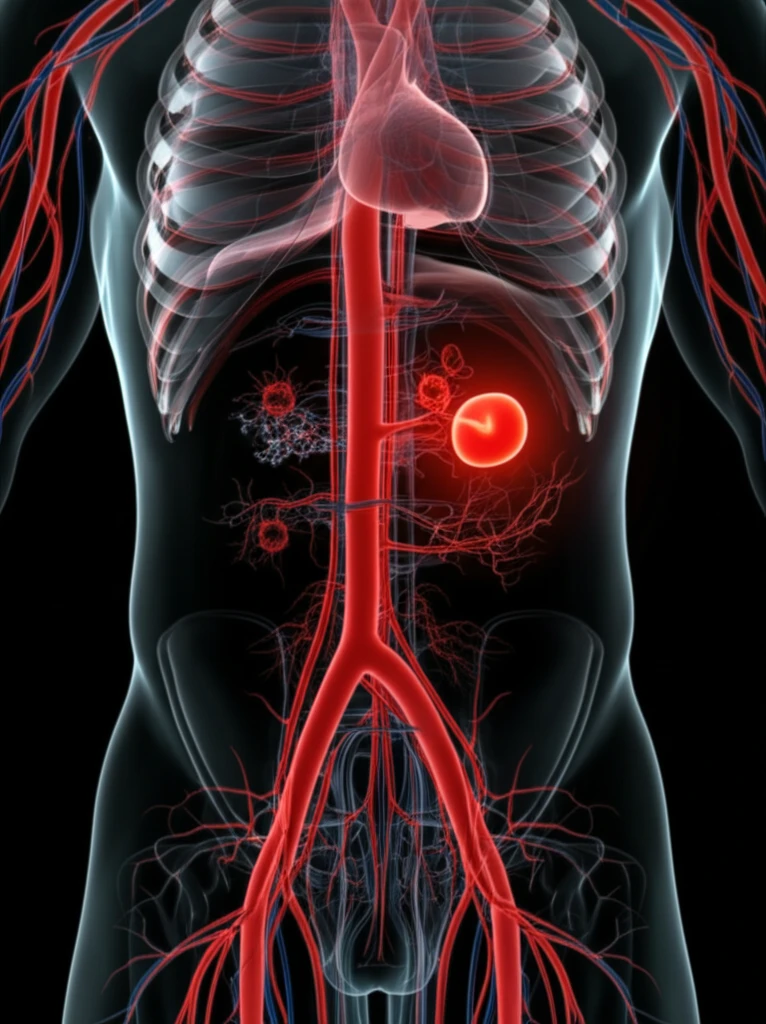
When DVT occurs in an unusual location, it raises critical questions about its origin. Unlike typical leg DVT, which is often linked to prolonged immobility or surgery, unusual sites suggest other factors are at play. Here's what different locations might indicate:
- Cerebral Veins: Thrombosis here can indicate a range of conditions, from infections to autoimmune disorders.
- Mesenteric Veins: Clots in these veins may point to intra-abdominal infections, inflammatory conditions, or even certain cancers.
- Upper Extremity Veins: Thrombosis in the arms can be associated with central venous catheters, thoracic outlet syndrome, or hypercoagulable states.
The Broader Significance: What Uncommon Clots Tell Us
The occurrence of DVT in unusual locations is relatively rare but serves as an important indicator of underlying health problems. Identifying the root cause requires a comprehensive approach, including detailed medical history, physical examination, and targeted diagnostic testing. This may involve imaging studies, blood tests for thrombophilia, and investigations for cancer or autoimmune disorders.
For instance, a study correlated D-dimer levels with the extent of thrombosis in lower limb DVT, suggesting that elevated D-dimer levels might indicate more extensive clots and a higher risk of pulmonary embolism. This highlights the potential for using biomarkers to assess the severity and guide management of DVT.
Ultimately, recognizing and understanding unusual DVT locations is crucial for early diagnosis and treatment of underlying conditions, improving patient outcomes and preventing potentially life-threatening complications.
