Unlocking the Mystery of Insulin Resistance: How a Tiny Molecule Impacts Your Health
"Researchers Discover a Key Mechanism Linking Glucocorticoids, Ceramides, and Insulin Resistance, Offering New Hope for Managing Metabolic Health."
In the complex world of health, understanding how our bodies use and respond to insulin is critical. Insulin resistance, a condition where cells become less responsive to insulin, is a major player in type 2 diabetes and cardiovascular diseases. But what drives this resistance? Recent research sheds light on a surprising link between a tiny molecule, a hormone, and how our bodies handle sugar.
This groundbreaking study, published in Science Signaling, delves into the role of glucocorticoids, hormones often produced during stress, and their effect on insulin resistance. The research highlights a specific protein, Angptl4, and its connection to ceramides, a type of fat molecule. This research opens new doors in how we approach conditions like diabetes, giving us a clearer picture of the underlying mechanisms at play.
This article breaks down this complex research, highlighting its relevance to your health. We will discuss how glucocorticoids influence insulin resistance, how Angptl4 and ceramides fit into the picture, and the potential implications of these findings for treatment and prevention.
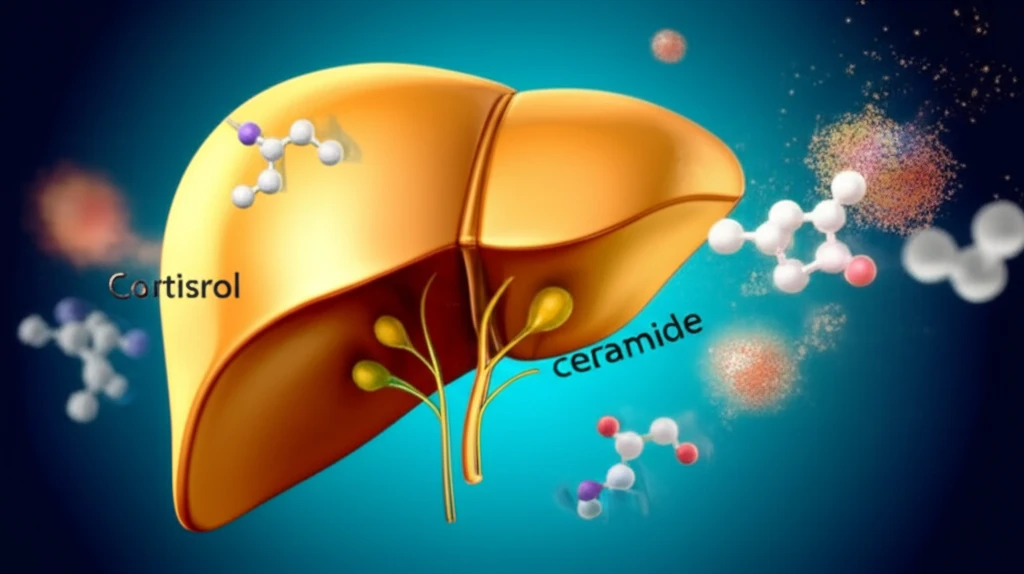
The Glucocorticoid-Ceramide Connection: Unraveling the Root Causes of Insulin Resistance
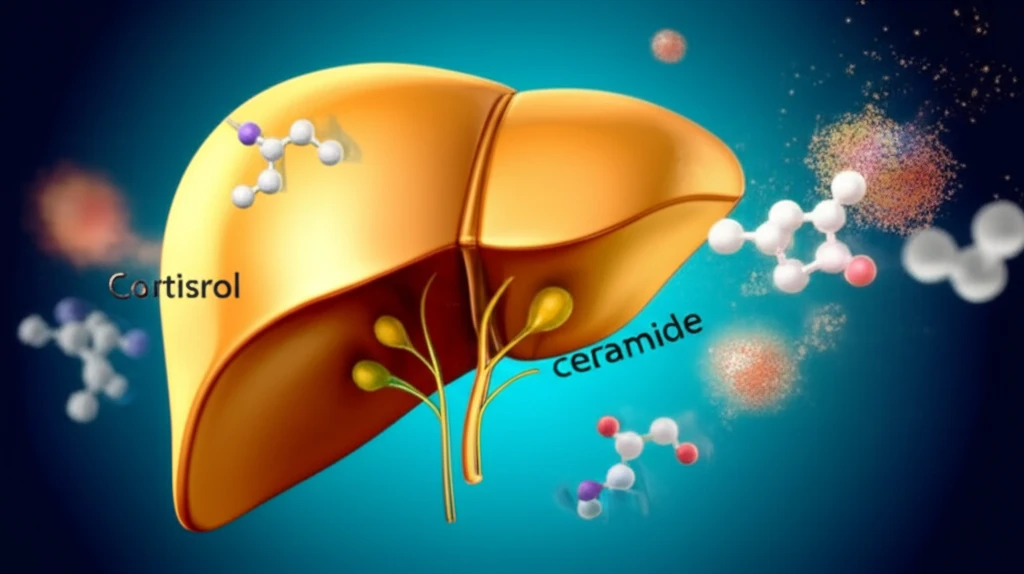
Glucocorticoids, like cortisol, are essential for managing stress and inflammation. However, long-term exposure to elevated levels of these hormones has been linked to insulin resistance. But the how? This research identifies the pivotal role of Angptl4, a protein previously associated with fat metabolism, as a key player.
- Glucocorticoid Exposure: Triggered by stress, and medications that can lead to insulin resistance.
- Angptl4 Production: A protein made by the body in response to glucocorticoids, this is like a messenger.
- Ceramide Buildup: Ceramides are a type of fat molecule that can impair insulin's function.
- Insulin Resistance: The body's cells become less receptive to insulin, resulting in elevated blood sugar levels.
Looking Ahead: New Insights and Opportunities
This research gives us a better insight into how stress, hormones, and fat metabolism impact insulin resistance. Further investigation of the ceramide pathways may result in novel therapies. These insights provide an improved perspective on how to approach disorders related to glucose regulation and suggest that modulating the ceramide pathway may be an effective approach to restore insulin sensitivity.
