Unlocking Sjögren's Syndrome: New Insights into Immune Imbalance and Potential Therapies
"Groundbreaking research sheds light on the complex immune dysregulation in Sjögren's Syndrome, paving the way for targeted treatments and improved patient outcomes."
Sjögren's Syndrome (pSS) is a chronic autoimmune disorder characterized by the immune system mistakenly attacking the body's moisture-producing glands. This primarily affects the salivary and lacrimal glands, leading to dry mouth and dry eyes, hallmark symptoms of the disease. However, pSS can also manifest in a variety of systemic ways, impacting joints, skin, nerves, and other organs, making diagnosis and management complex.
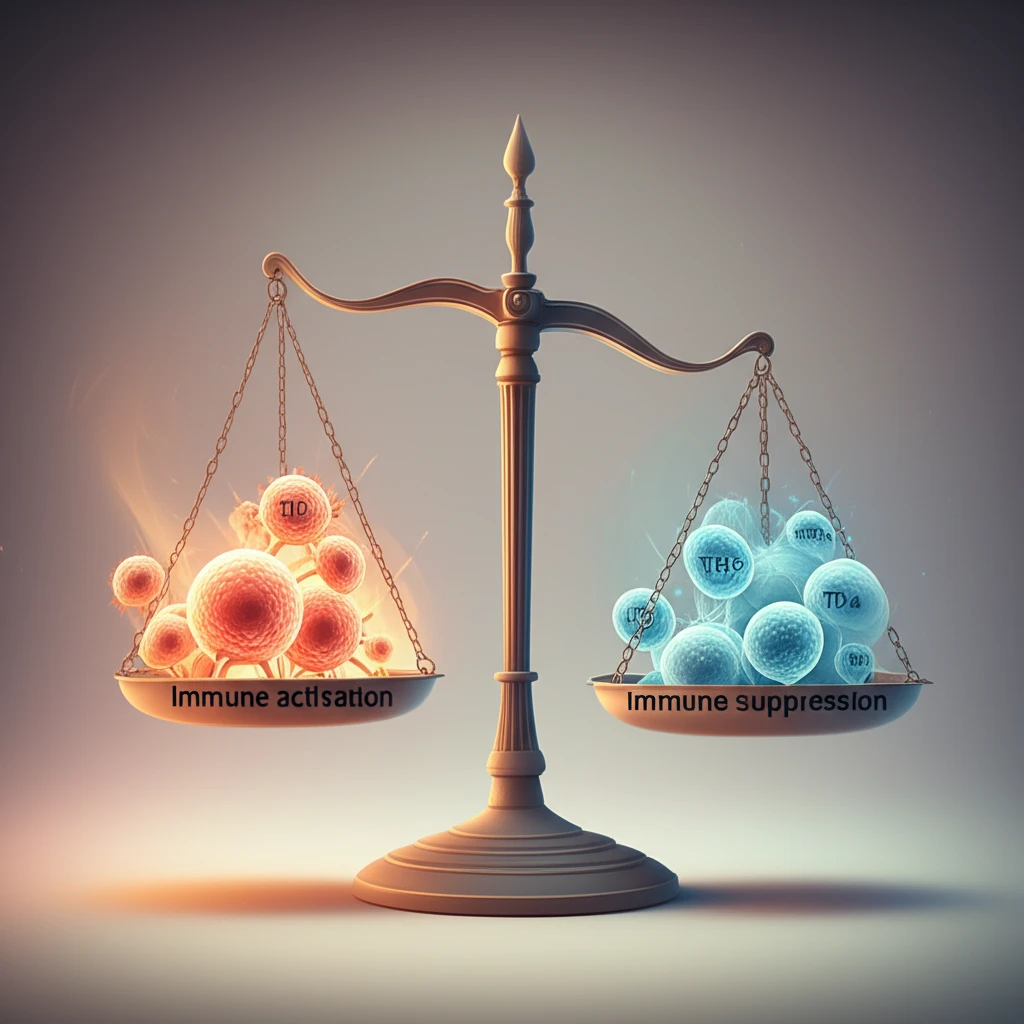
Recent research has significantly advanced our understanding of the intricate immune processes that drive pSS. These studies have illuminated the roles of various immune cells and molecular pathways, offering potential new avenues for targeted therapies. As our knowledge deepens, the possibility of more effective and personalized treatments for pSS comes into sharper focus.
This article explores key findings from recent scientific investigations into the immunological aspects of Sjögren's Syndrome. We will delve into the roles of specific immune cells like T follicular helper cells (Tfh), T follicular regulatory cells (Tfr), regulatory B cells (Breg), and innate lymphoid cells (ILC2), and how imbalances in these populations contribute to the disease. Further, we'll examine the potential therapeutic implications of these discoveries, offering hope for improved management of this challenging condition.
T Follicular Regulatory Cells: Balancing the Immune Response in Sjögren's Syndrome
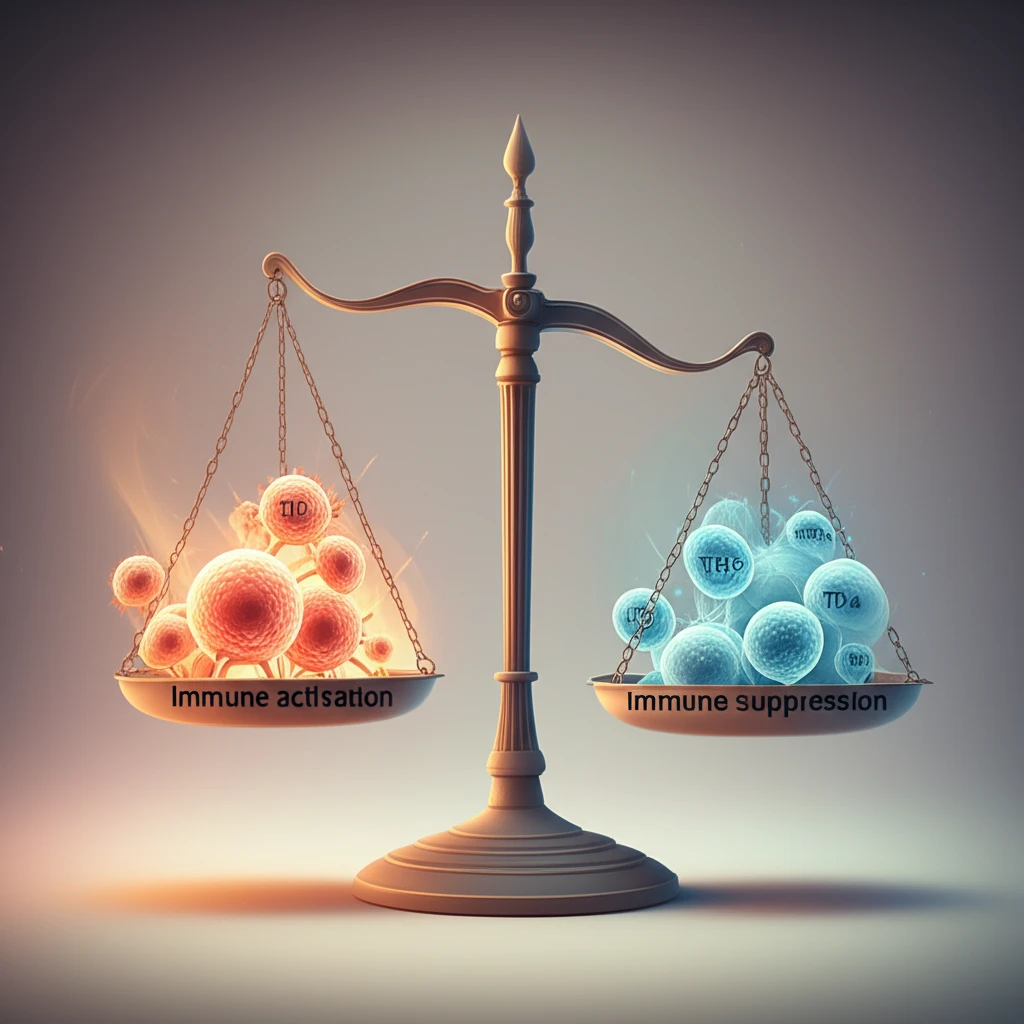
Within the intricate network of immune cells, T follicular helper (Tfh) cells play a crucial role in assisting B cells to produce antibodies. In pSS patients, the proportion of circulating Tfh cells is often elevated, correlating with higher disease activity. However, the counterbalance comes from T follicular regulatory (Tfr) cells, which help to control Tfh cell activity and maintain immune homeostasis.
- Increased Tfr Cell Numbers: pSS patients exhibit a higher proportion of Tfr cells, seemingly attempting to regulate the overactive immune system.
- Reduced CTLA-4 Expression: The key suppressive molecule CTLA-4 is significantly reduced on Tfr cells in pSS, impairing their functionality.
- Implications for B Cell Hyperactivity: The impaired suppressive capacity of Tfr cells may contribute to the expansion of Tfh cells and the subsequent hyperactivity of B cells, driving autoantibody production.
Restoring Immune Harmony: The Future of Sjögren's Syndrome Treatment
The insights gained from these studies highlight the potential for targeted therapies aimed at restoring immune balance in Sjögren's Syndrome. By understanding the specific defects in immune cell function and the dysregulation of key molecular pathways, researchers can develop more effective treatments that address the underlying causes of the disease, rather than merely managing the symptoms. As research continues, there is growing optimism that new and innovative therapies will transform the lives of individuals living with Sjögren's Syndrome.
