Uncommon Culprit, Common Symptoms: When Shoulder Pain Signals More Than Just Arthritis
"Discover how pyomyositis can mimic septic arthritis and why a high index of suspicion is crucial for early diagnosis and treatment."
Pyomyositis, while relatively uncommon, is often considered a tropical disease, with higher prevalence rates in regions like Africa and the South Pacific. However, it's increasingly being recognized in Western countries. Pyomyositis requires a high degree of suspicion due to its potential for misdiagnosis.
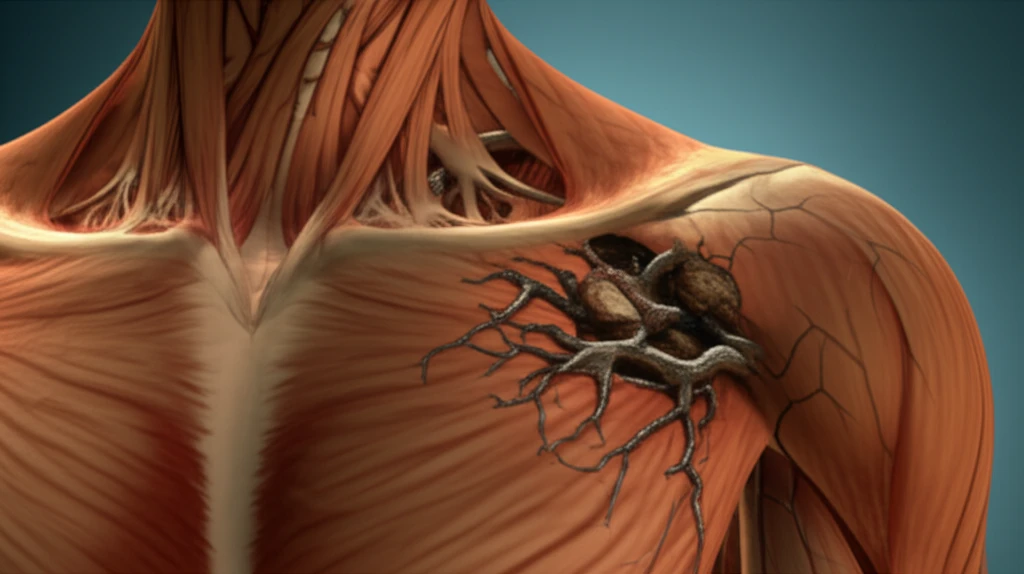
Pyomyositis is essentially a deep-seated bacterial infection affecting skeletal muscles, most frequently in the lower limbs, such as the quadriceps, hamstrings, gluteal muscles, and iliopsoas. While the exact cause is often unclear, several risk factors have been identified, including immunosuppression, intense physical exertion, and direct trauma to the muscle.
The challenge with pyomyositis is that it can easily be overlooked, either because it isn't considered in the initial differential diagnosis, or because patients present with nonspecific symptoms that mimic other conditions, such as septic arthritis. This can delay appropriate treatment and potentially lead to complications.
Case Study: A Diagnostic Puzzle
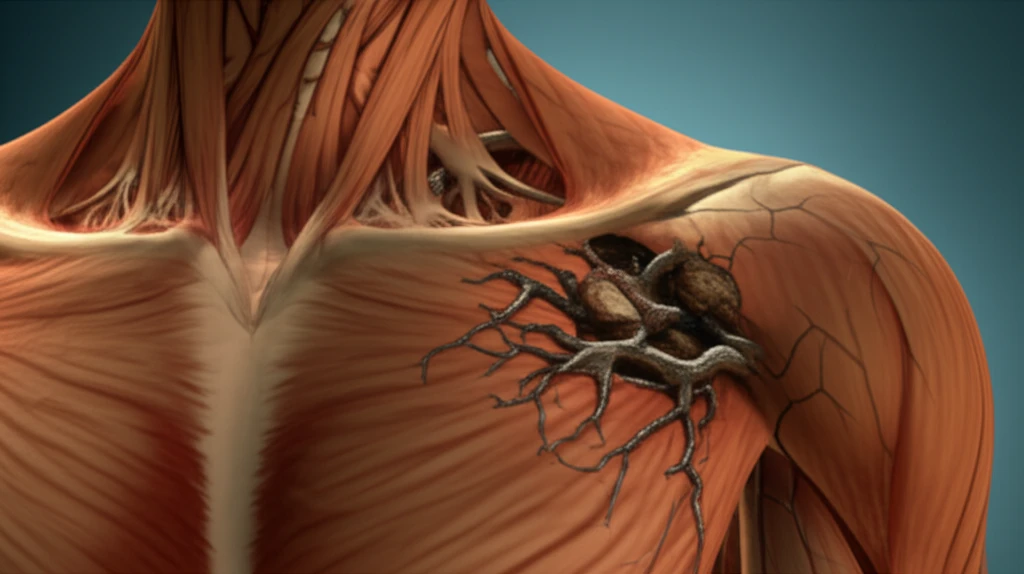
Consider the case of Mrs. ET, a 54-year-old woman who presented with a two-week history of progressive, dull aching pain in her right shoulder. Her symptoms had worsened in the days leading up to her admission, accompanied by fever, rigors, and significant pain with even minimal shoulder joint movement. Her medical history was unremarkable, except for hypertension. There were no indications of diabetes, immunosuppression, or any recent trauma.
- White cell count (WCC): 9.62 × 109/L
- Neutrophils: 8.73 × 109/L
- C-reactive protein (CRP): 52 mg/L
The Takeaway: Think Beyond the Obvious
Mrs. ET's case underscores the importance of maintaining a broad differential diagnosis, even when initial presentations suggest common conditions. Pyomyositis, though rare, should be considered in patients presenting with shoulder pain and signs of sepsis, even in the absence of typical risk factors. Early diagnosis, coupled with appropriate antibiotic therapy and, if necessary, surgical intervention, can lead to favorable outcomes and prevent serious complications.
