The Role of Complement Activation in Autoimmune Diseases: New Insights and Therapeutic Potential
"Exploring the Links Between Complement Pathways, Lupus Nephritis, and Pulmonary Hypertension."
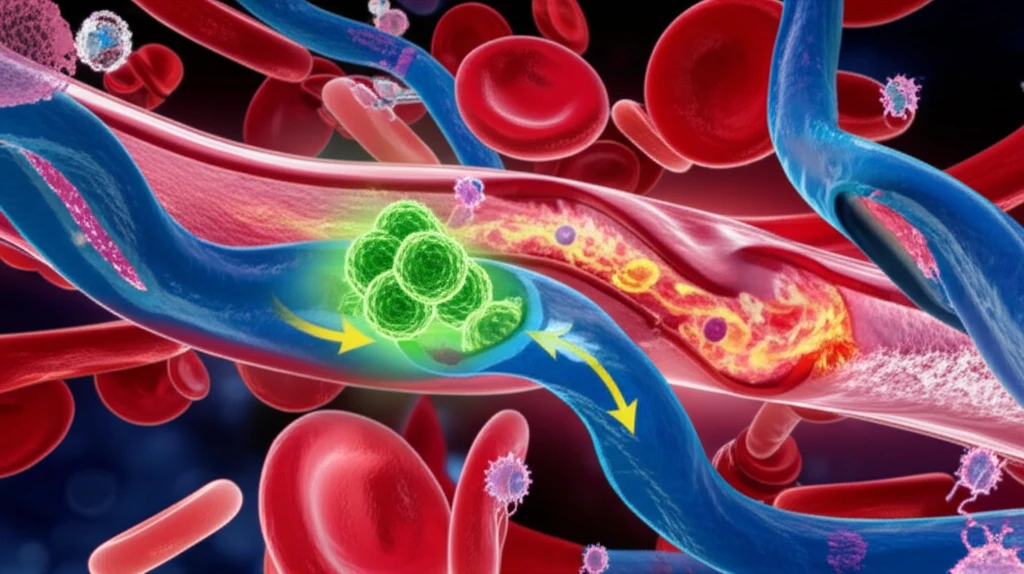
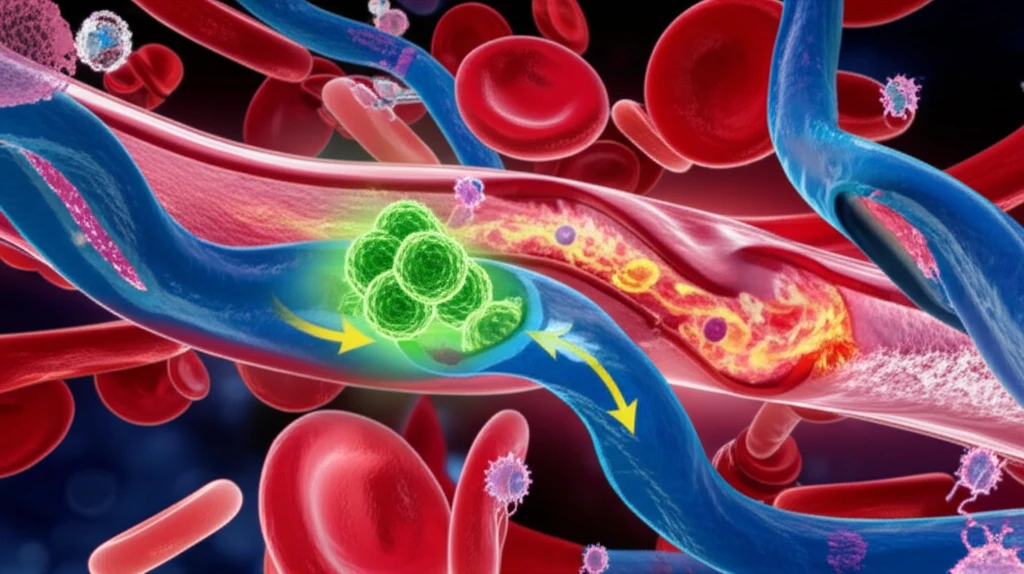
Autoimmune diseases, such as systemic lupus erythematosus (SLE), are characterized by the immune system mistakenly attacking the body's own tissues and organs. A key player in this process is the complement system, a part of the immune system that enhances (complements) the ability of antibodies and phagocytic cells to clear microbes and damaged cells from an organism, promote inflammation, and attack the pathogen's cell membrane. However, when dysregulated, the complement system can contribute to the pathology of autoimmune diseases.
One area of significant research interest is the role of the alternative complement pathway in lupus nephritis (LN), a kidney inflammation caused by SLE. Previous studies have suggested that excessive activation of this pathway, especially in the absence of factor H (a regulator of complement activity) or functional impairment, is a key factor in the development of LN. Furthermore, the connection between pulmonary hypertension (PH), a condition of high blood pressure in the arteries to the lungs, and LN has also garnered attention, with vasculopathy (disease of the blood vessels) emerging as a critical link.
Recent research has delved deeper into the clinical and pathological significance of alternative complement activation in patients with both pulmonary hypertension and lupus nephritis. By analyzing patient data, detecting complement components, and examining lung specimens, researchers aim to unravel the complex interplay between complement activation, vascular lesions, and the severity of these conditions.
How Does Complement Activation Contribute to Pulmonary Hypertension in Lupus Nephritis?
A study was conducted analyzing patients with and without pulmonary hypertension in the context of lupus nephritis. Plasma samples were analyzed for ANCA (anti-neutrophil cytoplasmic antibodies) and major complement components. Lung specimens from patients with both PH and LN were examined using immunofluorescence staining to detect the presence of Bb, C3d, and C5b-9, which are markers of complement activation.
- Complement Levels: Higher levels of Bb (a component of the alternative pathway) and lower levels of factor H (a complement regulator) were found in patients with pulmonary hypertension.
- Clinical Manifestations: The pulmonary hypertension group exhibited a higher incidence of thrombocytopenia (low platelet count) and lower rates of malar rash, alopecia (hair loss), and arthritis.
- Laboratory Findings: Patients with pulmonary hypertension and lupus nephritis had lower hemoglobin levels and higher D-Dimer levels (indicating blood clot formation). There were also higher ratios of anti-RNP and anti-cardiolipin antibodies in the lupus nephritis group.
- Lung Pathology: The deposition of Bb in lung tissues was associated with the severity of lung injury.
Implications and Future Directions
This study provides additional evidence that complement activation through the alternative pathway is a key factor in the development of pulmonary hypertension in the context of lupus nephritis. Understanding the specific mechanisms by which complement contributes to vascular lesions may pave the way for targeted therapies aimed at modulating complement activity and preventing the progression of these debilitating conditions. By targeting the alternative complement pathway, clinicians may be able to improve renal outcomes and overall prognosis for patients with pulmonary hypertension and lupus nephritis.
