TBS Unlocked: Is This Bone Density Secret Key to Fracture Risk?
"Beyond BMD: How Trabecular Bone Score (TBS) is changing osteoporosis evaluation and FRAX scores."
For years, bone mineral density (BMD) scans have been the go-to for predicting fracture risk. Yet, many individuals with fractures show BMD values within the normal or osteopenic range. This is because BMD only tells part of the story. Bone quality, specifically its microarchitecture, plays a crucial role in bone strength.
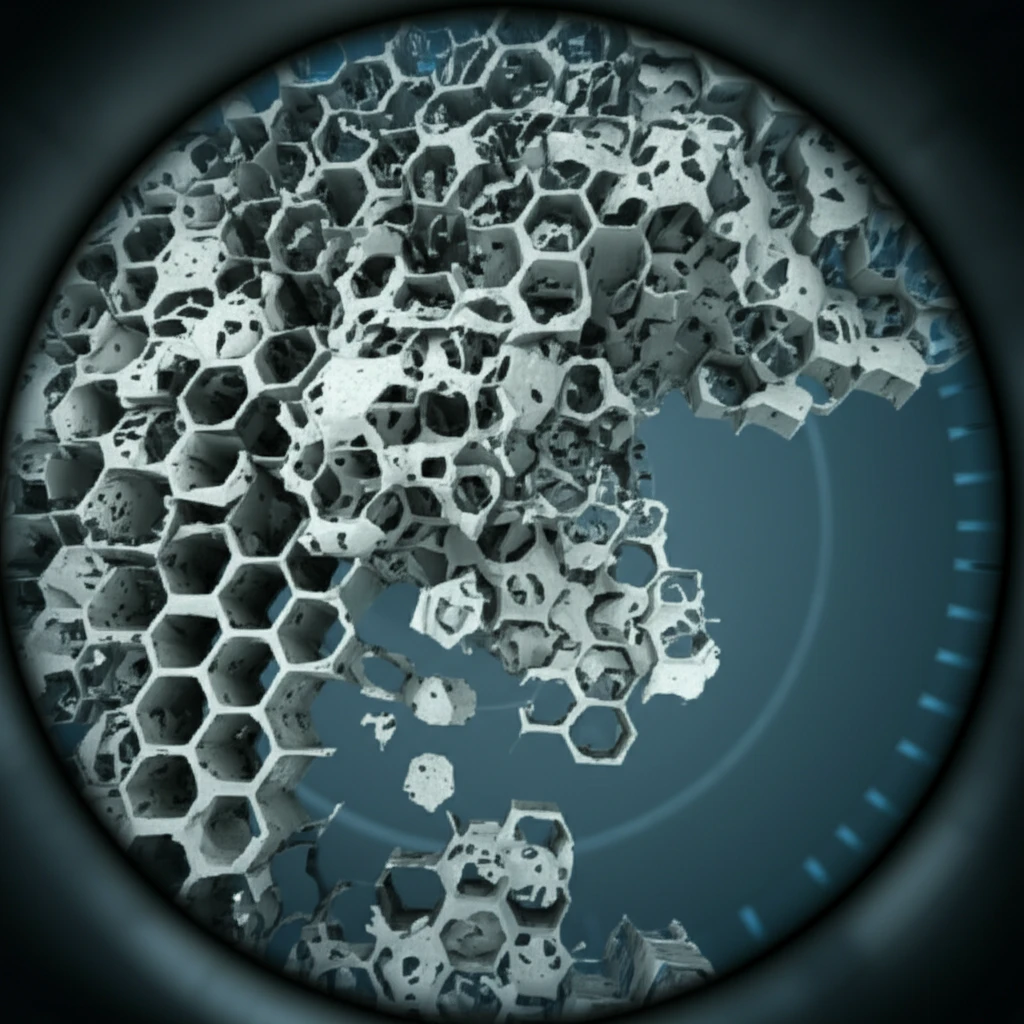
Enter Trabecular Bone Score (TBS), a technique designed to assess image texture from standard spine DXA scans, providing insights into skeletal quality that are partially independent of BMD. Think of it as a way to 'read' the subtle patterns within your bones that BMD might miss. In 2012, the U.S. Food and Drug Administration (FDA) approved TBS as a tool related to bone microarchitecture and fracture risk assessment.
This article dives into the world of TBS, exploring its development, validation, clinical applications, and how it's reshaping our understanding and management of osteoporosis.
TBS: How It Works & What It Reveals
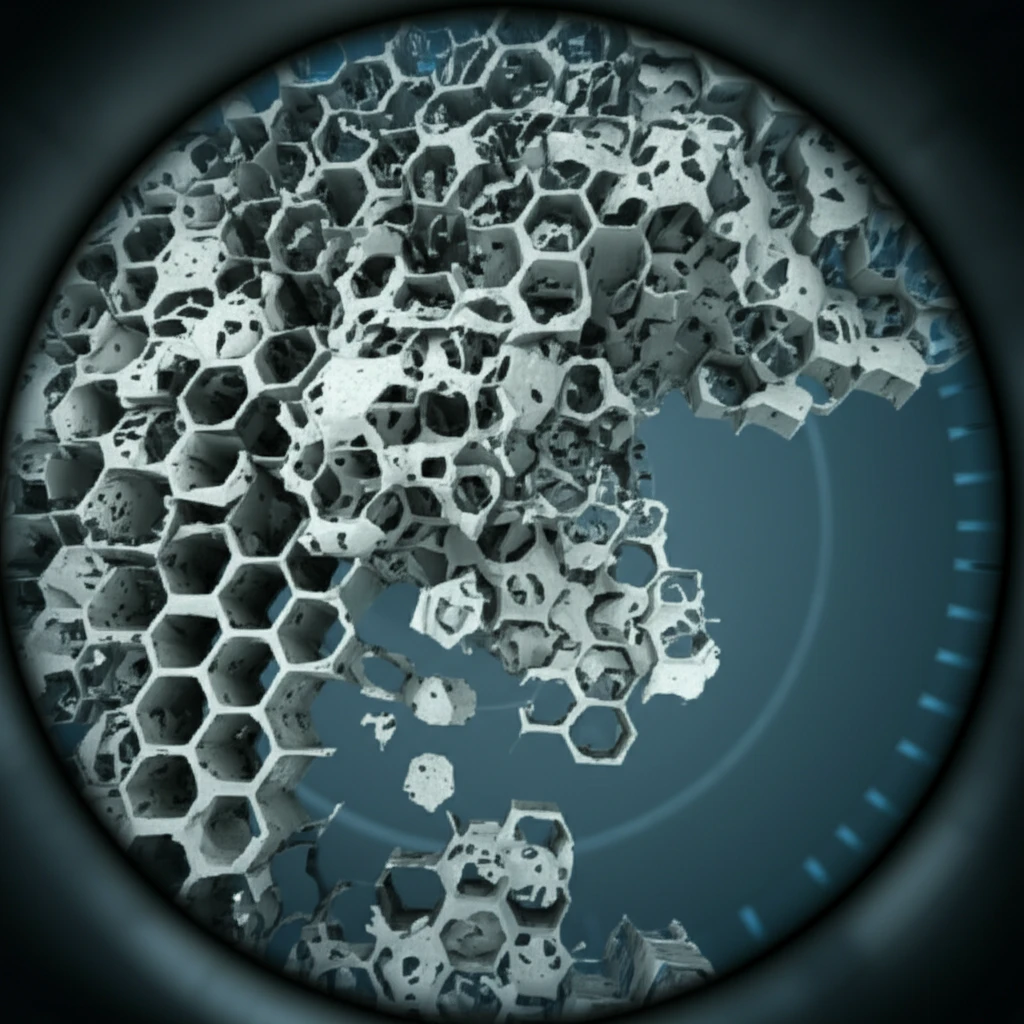
TBS leverages the information already captured in standard dual-energy X-ray absorptiometry (DXA) images of the lumbar spine. It analyzes the variations in gray levels within the image, using a mathematical approach called a variogram. The result is a score that reflects the homogeneity of the bone's texture.
- Higher TBS Values: Indicate a more homogenous, well-connected trabecular structure, generally associated with stronger bones.
- Lower TBS Values: Suggest a less well-organized, potentially weaker bone structure with reduced trabecular connectivity.
TBS: A Clinically Useful Tool
While TBS doesn't directly measure bone microarchitecture, research has consistently demonstrated its clinical utility as a fracture risk prediction tool. Studies show that lower TBS values are associated with an increased risk of osteoporotic fractures, independent of BMD.
Combining TBS with FRAX (Fracture Risk Assessment Tool) significantly enhances fracture risk prediction, particularly for individuals near a treatment threshold. This allows clinicians to make more informed decisions about interventions, especially when FRAX scores alone are inconclusive.
Lumbar spine TBS is a recently developed image-based software technique for skeletal assessment, complementary to conventional BMD, which has been shown to be clinically useful as a fracture risk prediction tool. Recent and ongoing studies are helping to refine the clinical utility of TBS.
