Syncope and Pulmonary Embolism: What You Need to Know About This Risky Combination
"New research reveals the surprising link between fainting spells and dangerous blood clots, highlighting who's most at risk and how to protect yourself."
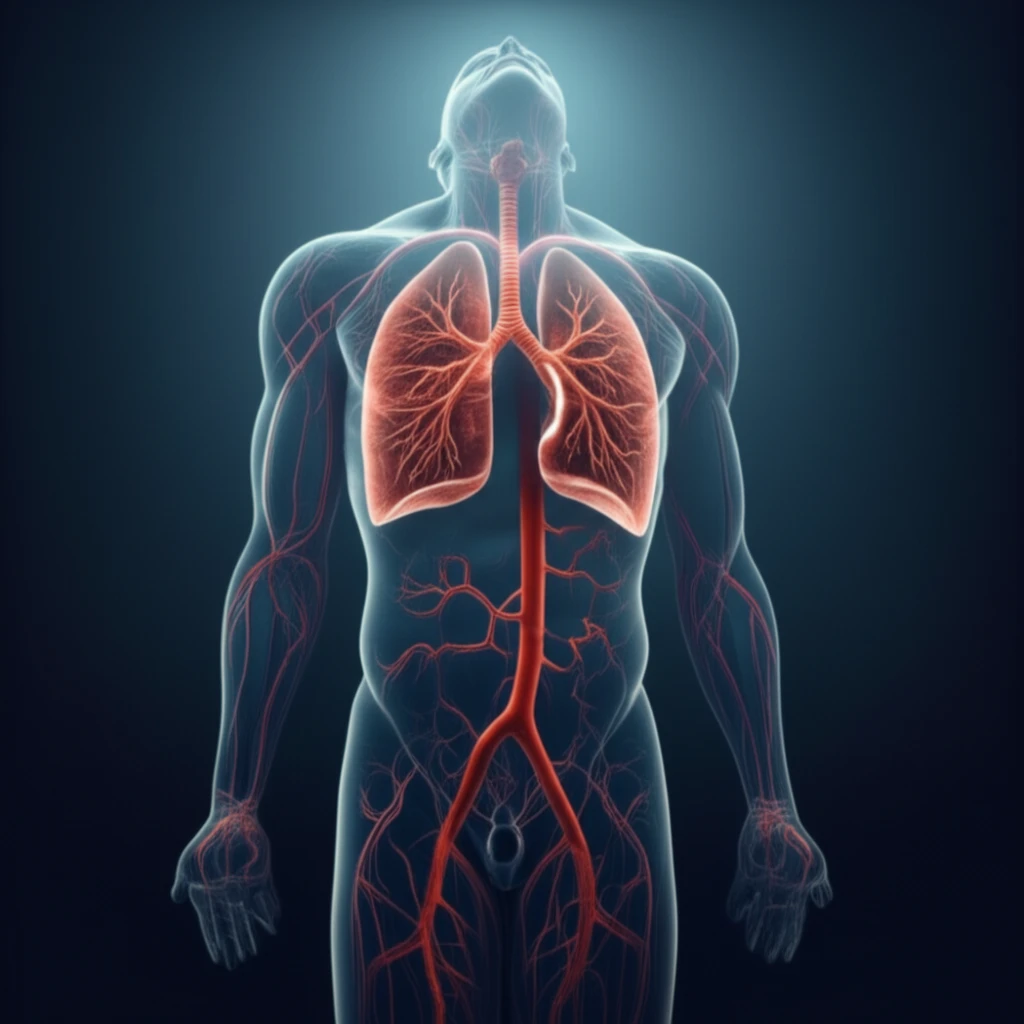
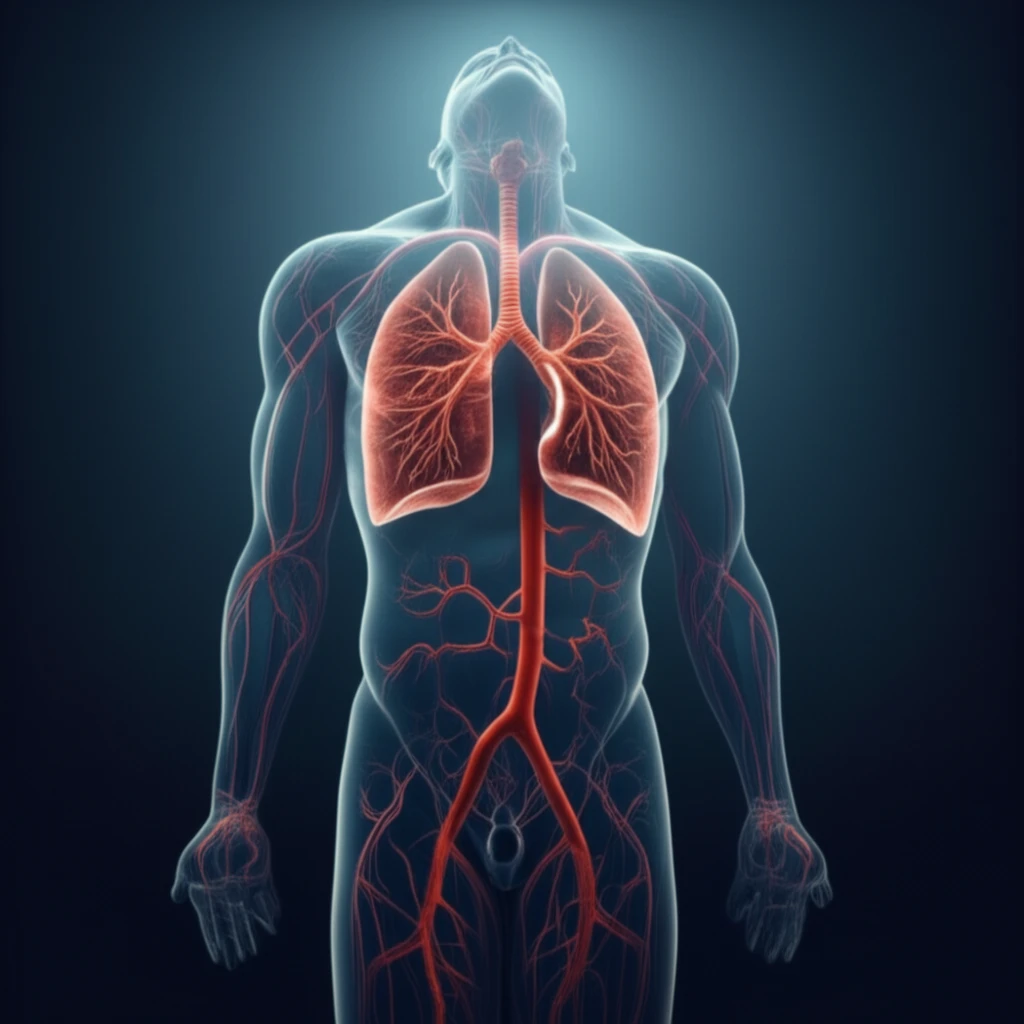
That dizzy spell, the sudden blackout—syncope, or fainting, is something most people experience at least once. Usually, it’s harmless, maybe a sign of dehydration or low blood sugar. But what if that faint was a warning sign of something far more serious, like a pulmonary embolism (PE), a life-threatening blood clot in the lungs? It sounds scary, and it is, but understanding the connection is the first step to protecting yourself and your loved ones.
Pulmonary embolism is a serious condition where blood clots block the arteries in your lungs. It can cause shortness of breath, chest pain, and even death. Syncope has long been recognized as a potential symptom of PE, but the relationship isn't always clear. Is syncope simply a sign of a more severe PE, or does it independently increase the risk? Recent research is shedding light on this complex issue, providing vital information that could save lives.
This article breaks down the latest findings, translating complex medical research into easy-to-understand language. We'll explore the link between syncope and PE, who is most at risk, and what steps you can take to stay informed and advocate for your health. It's about empowering you with knowledge so you can recognize the warning signs and seek help when it matters most.
The Syncope-PE Connection: Unpacking the Risks
A recent study published in the European Heart Journal delved into this very question. Researchers conducted a meta-analysis, pooling data from 29 studies involving nearly 22,000 patients with pulmonary embolism. Their goal was to determine if syncope was associated with worse outcomes in PE patients.
- Hemodynamic Instability: This means problems with blood pressure and blood flow, indicating a more severe PE.
- Right Ventricular Dysfunction: The right ventricle is a chamber of the heart that pumps blood to the lungs. PE can strain this chamber, leading to dysfunction.
- Higher Risk of Early Death: Syncope was linked to an increased risk of death within the first 30 days of the PE diagnosis.
What Does This Mean for You? Taking Control of Your Health
The key takeaway is that syncope in the context of pulmonary embolism shouldn't be ignored. If you experience syncope along with symptoms like shortness of breath or chest pain, seek immediate medical attention. It's also crucial to inform your doctor about any history of syncope, as this information can help them assess your risk and make informed decisions about your care. While more research is always needed, understanding the potential link between syncope and PE empowers you to be a more informed and proactive advocate for your own health.
