Stroke Treatment Showdown: Is Combining Therapies Better Than One?
"A new look at how combining intra-arterial thrombolysis (IAT) with mechanical thrombectomy (MT) could change stroke treatment outcomes."
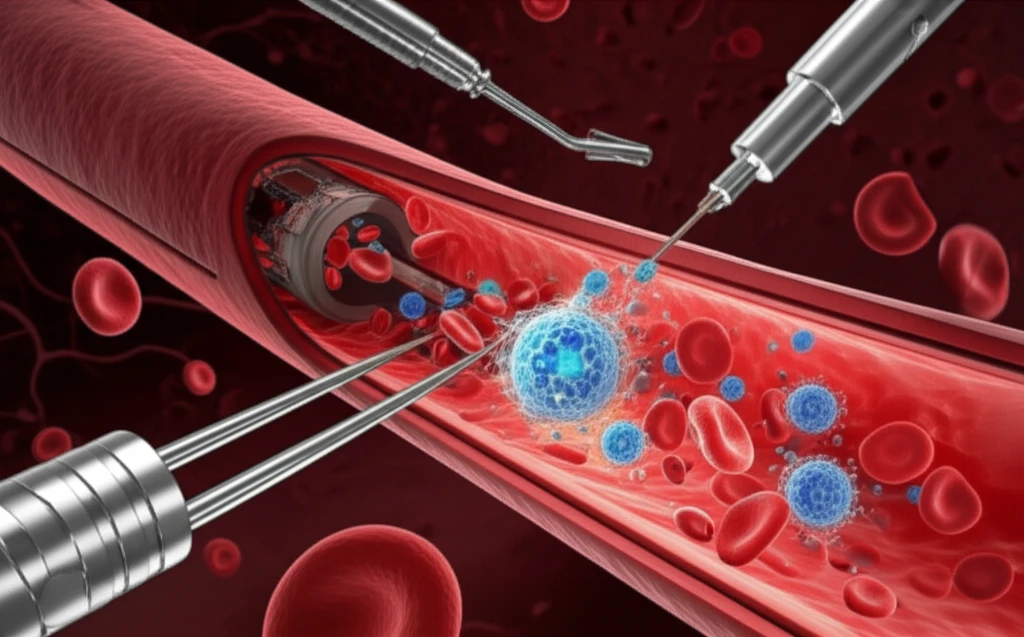
Stroke is a leading cause of disability, and rapid treatment is critical. For many patients suffering from acute ischemic stroke, endovascular interventions, which involve treating the stroke from inside the blood vessels, offer a lifeline.
Among these interventions, mechanical thrombectomy (MT) has become a standard approach, particularly for those ineligible for or unresponsive to intravenous thrombolysis (clot-busting drugs). However, the role of combining MT with intra-arterial thrombolysis (IAT), where clot-busting drugs are delivered directly to the site of the blockage, has remained a topic of investigation.
A retrospective study has shed new light on the potential benefits of this combined approach, comparing outcomes of patients who received MT alone versus those who underwent combined MT and IAT. The results offer valuable insights into improving stroke care and patient recovery.
IAT and MT Combination: A Closer Look at Stroke Treatment
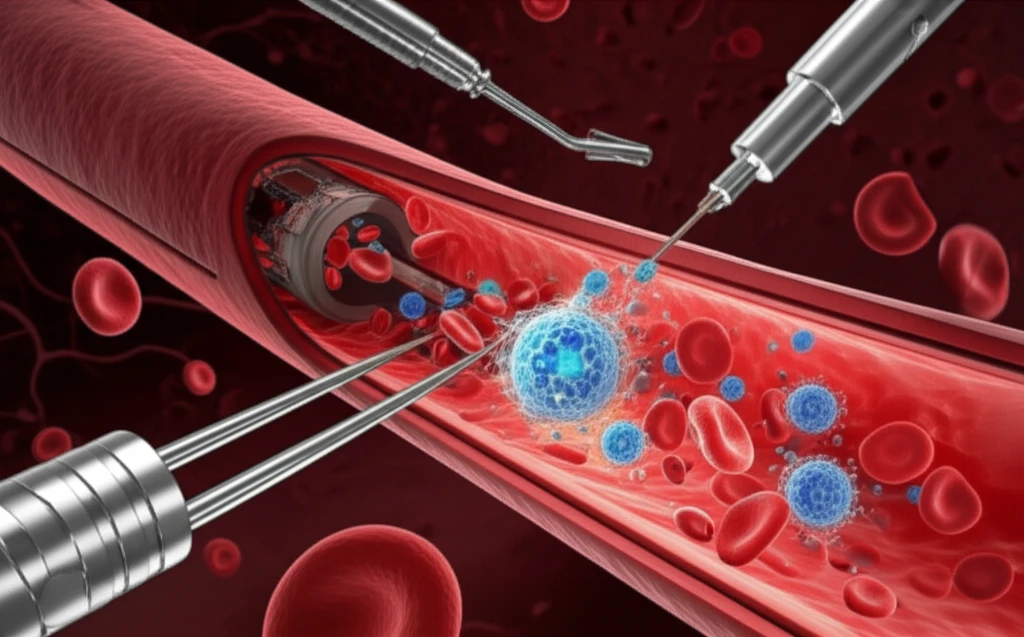
The study, conducted at a comprehensive stroke center, retrospectively reviewed the cases of 200 patients who underwent endovascular treatments for acute ischemic stroke between 2007 and 2011. Out of these, 115 patients met the inclusion criteria for comparison: one group received MT alone, while the other received a combination of MT and IAT. The researchers then analyzed various outcome parameters to assess the safety and efficacy of each approach.
- Discharge NIHSS (National Institutes of Health Stroke Scale): A measure of neurological deficit.
- Clinical improvement: Defined as a decrease of more than 4 points on the NIHSS.
- TIMI 2-3 (Thrombolysis in Myocardial Infarction) flow: Indicating partial to complete recanalization or restoration of blood flow.
- Discharge modified Rankin Scale (mRS) ≤3: Assessing functional independence, with a score of 3 or less indicating a better outcome.
- Symptomatic Intracerebral Hemorrhage (ICH): Bleeding in the brain causing new or worsening neurological symptoms.
- All-cause mortality: Death from any cause.
Interpreting the Findings: Risks and Rewards
While the study suggests potential advantages of the combined approach, it also reported higher rates of hemorrhage and slightly increased mortality rates in the combined therapy group. These findings underscore the need for careful patient selection and meticulous execution of the combined technique. Further research, including larger, randomized controlled trials, is essential to validate these findings and refine treatment protocols. In the meantime, this study provides valuable insights for clinicians to consider when making treatment decisions for acute ischemic stroke patients.
