Smarter Cancer Treatment: How Nanotechnology Can Overcome Drug Resistance
"Revolutionary reduction-sensitive micelles target tumor cells, reversing multidrug resistance and paving the way for more effective, personalized cancer therapies."
Chemotherapy, while a cornerstone of cancer treatment, often faces a significant hurdle: multidrug resistance (MDR). Cancer cells can develop the ability to resist the effects of drugs designed to kill them, rendering treatments ineffective. This resistance stems from various mechanisms, including increased drug efflux, reduced drug uptake, and alterations in drug targets within the cancer cells. Overcoming MDR is, therefore, crucial to improving cancer treatment outcomes.
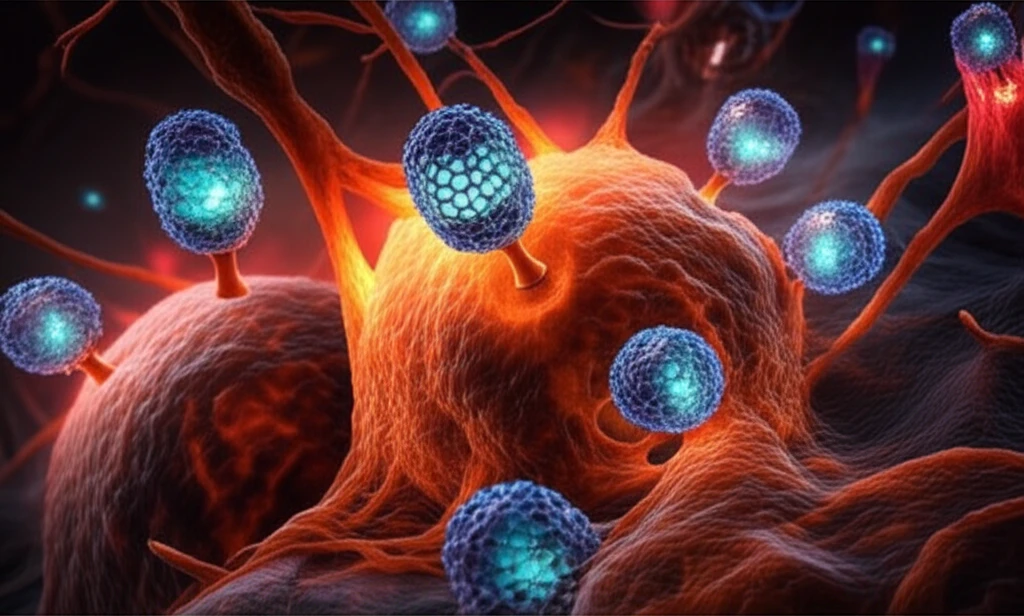
To combat MDR, scientists are increasingly turning to nanotechnology. Nanocarriers, tiny vehicles designed to deliver drugs directly to cancer cells, offer a promising avenue for enhancing treatment efficacy and reducing side effects. Among these nanocarriers, mixed micelles—self-assembling structures formed from different types of polymers—have garnered considerable attention.
Recent research has focused on developing reduction-sensitive mixed micelles that can selectively release their drug payload inside tumor cells. These micelles are engineered to respond to the unique reducing environment within cancer cells, triggering drug release and overcoming resistance mechanisms. By combining reduction sensitivity with active targeting capabilities, these innovative nanocarriers hold the potential to revolutionize cancer therapy.
The Science Behind Reduction-Sensitive Mixed Micelles
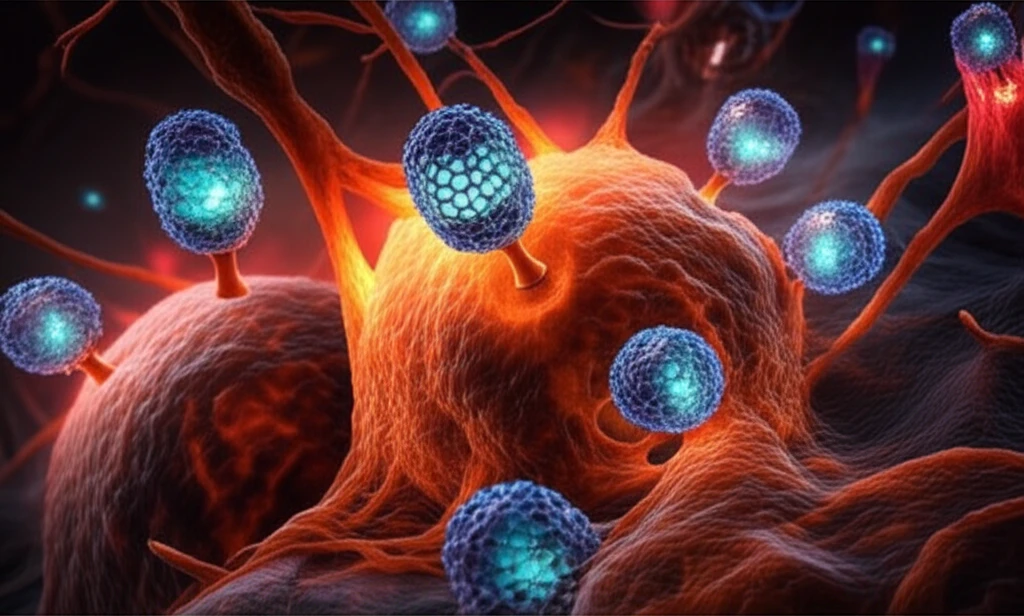
At the heart of this advancement lies the design and synthesis of reduction-sensitive mixed micelles. These micelles are typically composed of two main components: a hyaluronic acid-poly(lactide) (HA-ss-PLA) conjugate and D-α-tocopheryl polyethylene glycol 1000 succinate (TPGS). The HA-ss-PLA conjugate provides both a targeting mechanism and reduction sensitivity, while TPGS aids in drug encapsulation and MDR reversal.
- Selective Targeting: Hyaluronic acid (HA) targets cancer cells that overexpress the CD44 receptor, ensuring that the micelles preferentially accumulate at the tumor site.
- Reduction Sensitivity: The disulfide bond (ss) in HA-ss-PLA is cleaved in the reducing environment of cancer cells, triggering the release of the encapsulated drug.
- MDR Reversal: TPGS acts as a P-glycoprotein (P-gp) efflux inhibitor, preventing cancer cells from pumping the drug out, thereby enhancing its intracellular concentration.
Future of Cancer Therapy: Targeted and Personalized Approaches
The development of reduction-sensitive mixed micelles represents a significant step forward in cancer therapy. By selectively targeting tumor cells and overcoming drug resistance mechanisms, these nanocarriers hold the potential to improve treatment outcomes and reduce side effects. The success of these micelles in delivering paclitaxel highlights their versatility and applicability to a wide range of chemotherapeutic drugs.
Looking ahead, further research is needed to optimize the design and formulation of mixed micelles for different types of cancer. Tailoring the targeting ligands and drug payloads to specific tumor characteristics will enable more personalized and effective treatment strategies. Additionally, clinical trials are essential to evaluate the safety and efficacy of these nanocarriers in human patients.
Ultimately, the integration of nanotechnology into cancer therapy promises a future where treatments are more targeted, efficient, and less toxic. As scientists continue to refine and innovate in this field, the dream of conquering cancer with personalized nanomedicine moves closer to reality.
