Rare Case Connection: When Bone Tumors and Adrenal Gland Tumors Collide
"Unveiling the Unusual Link Between Multicentric Giant Cell Tumors of Bone and Paraganglioma: A Case Report Analysis."
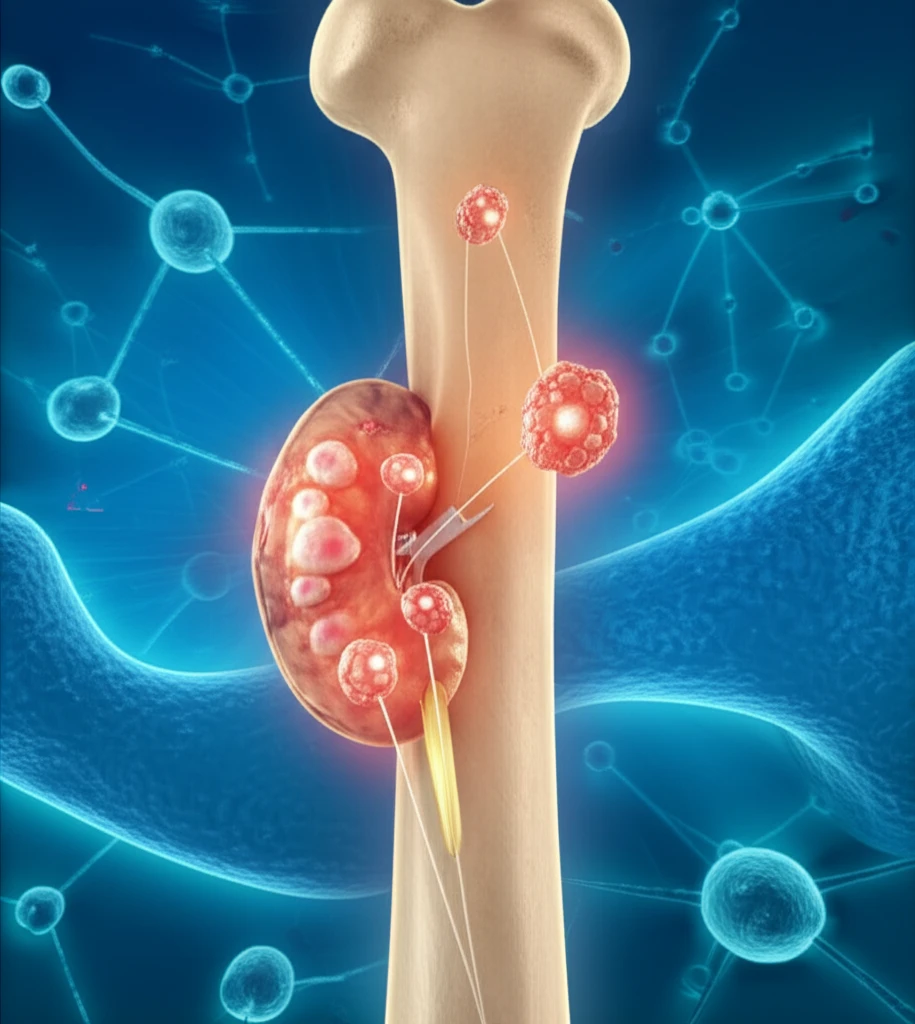
Giant cell tumors (GCTs) of bone, while relatively uncommon, typically account for a small percentage of primary bone tumors. These tumors occasionally metastasize, most frequently to the lungs. Recent research highlights the role of the RANKL pathway in GCT development, yet the precise mechanisms remain unclear.
Multicentric giant cell tumors (MGCTs), where tumors appear in multiple locations within the bone, are an even rarer occurrence. A recent case involving a young man diagnosed with both MGCT and a paraganglioma, a tumor of the adrenal glands, has presented an unusual opportunity to study the potential connections between these rare conditions.
This article delves into the details of this unique case report, exploring the clinical presentation, diagnostic process, treatment strategies, and potential underlying mechanisms that may link MGCT and paraganglioma. It offers insights into the complexities of rare tumor occurrences and emphasizes the importance of considering unusual associations in diagnosis and treatment planning.
The Case: A Young Man's Journey with MGCT and Paraganglioma
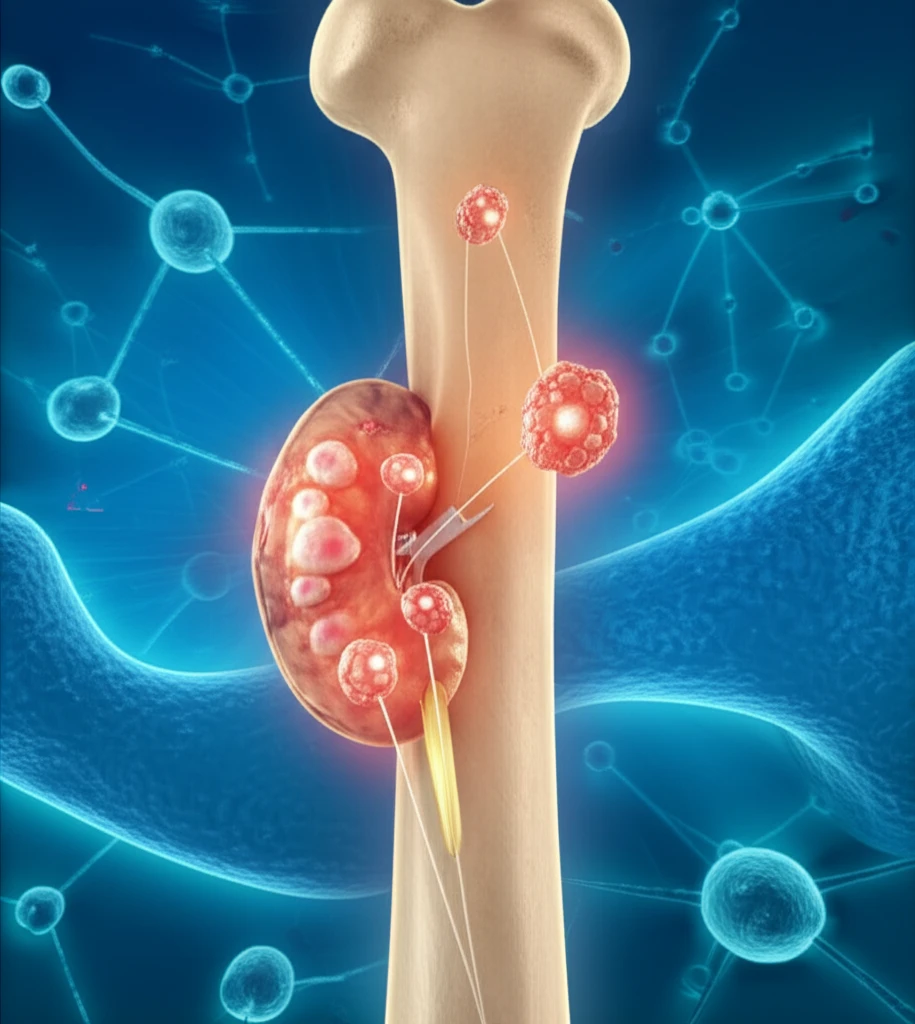
A 20-year-old male presented with recurrent pain in his left knee. Initial radiographs revealed lytic lesions with trabeculation and cortical thinning in the distal femur, proximal tibia and fibula, and distal ipsilateral tibia. These findings suggested multiple tumor sites, leading to a diagnosis of MGCT.
- Initial Presentation: Knee pain and multiple bone lesions.
- Diagnosis: MGCT confirmed, along with retroperitoneal paraganglioma and lung metastasis.
- Treatment: Surgical interventions for bone lesions and retroperitoneal tumor.
- Complications: Development of liver metastasis from the paraganglioma and further spread of GCT.
Unraveling the Connection and Implications for Future Research
The co-occurrence of MGCT and paraganglioma in this case is exceptionally rare, with limited existing literature on the topic. While a causal relationship cannot be definitively established, the observed correlation between the activity of the fibular GCT lesion and the status of the paraganglioma suggests a potential functional link.
The case highlights the importance of considering unusual associations in patients presenting with rare tumors. Further research is needed to investigate the potential underlying mechanisms that may connect MGCT and paraganglioma. One possible mechanism involves the role of beta-adrenoreceptor agonists, such as norepinephrine, in stimulating RANKL expression and promoting osteoclast differentiation.
This unique case report contributes to the growing body of knowledge on rare tumor occurrences and emphasizes the need for continued research to improve our understanding of these complex conditions. Further investigation into the potential link between MGCT and paraganglioma may lead to improved diagnostic and therapeutic strategies for patients with these rare tumors.
