Precision Dose: How New Methods Are Improving Cancer Therapy
"Dosimetry procedures for organs-at-risk in peptide receptor radionuclide therapy with lutetium-177 are transforming cancer treatment."
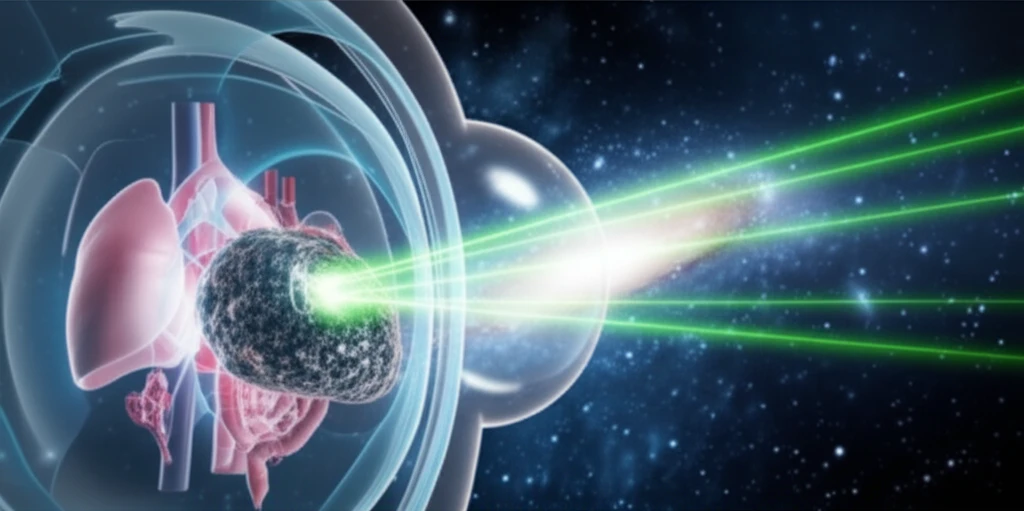
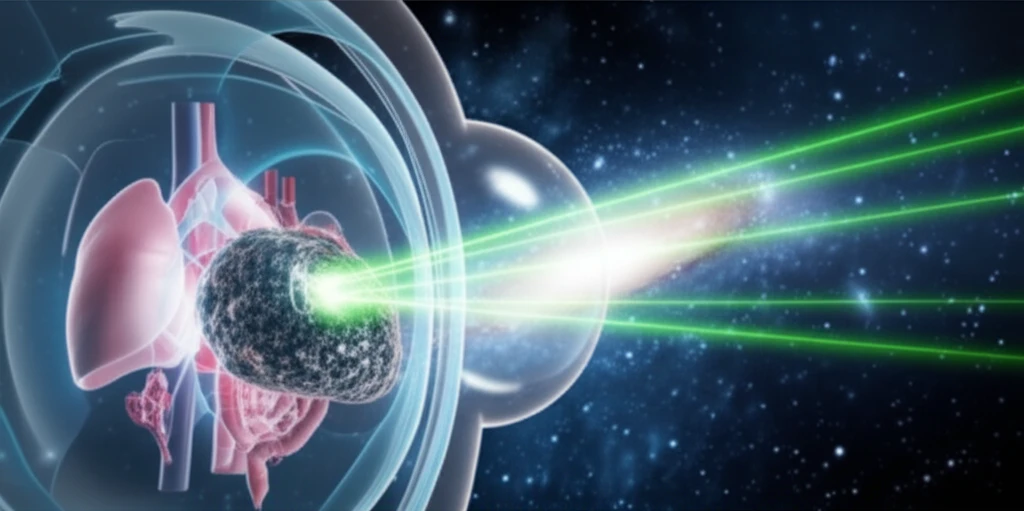
Molecular radiotherapy (MRT) is increasingly relying on precise dosimetry to tailor treatments and improve outcomes. Standardizing dosimetry procedures is crucial for maximizing therapeutic benefits and minimizing harm. A key challenge lies in determining the optimal range of absorbed doses that effectively target tumors while safeguarding organs-at-risk (OAR).
Developing standardized dosimetry methods in molecular radiotherapy presents multifaceted challenges, encompassing drug administration, data acquisition, activity quantification, and absorbed dose computation. Each step introduces variables that impact the accuracy and reproducibility of results. Effective implementation requires careful consideration of patient burden, practicality, cost-effectiveness, and the reliability of obtained data.
In the context of lutetium-177 (¹⁷⁷Lu) peptide receptor radionuclide therapy (PRRT), various approaches have been explored to refine dosimetry. These include phantom studies for improved imaging, adjustments to time-point measurements, kinetic and radiobiological modeling, and organ- and voxel-scale dosimetry based on Monte Carlo simulations. This article will discuss how these strategies improve cancer therapy.
Enhancing Precision in Dosimetry: A Multi-Step Approach
A recent study detailed a dosimetry procedure for organs-at-risk during ¹⁷⁷Lu-DOTATATE therapy, involving 47 patients with neuroendocrine tumors (NETs). The process integrates SPECT/CT imaging with blood sample analysis to enhance accuracy and minimize patient discomfort.
- Drug Administration: Administering lutetium-177 based radiopharmaceuticals.
- Data Acquisition: Serial SPECT/CT images were obtained at 4, 24, and 168 hours post-injection. Blood samples were taken at similar time points, along with additional samples within the first hour to capture early clearance.
- Activity Quantification: PMOD software was used to measure volumes and activity concentrations in kidneys, spleen, liver, red marrow, and the remainder of the body, using volumes of interest (VOIs) on SPECT/CT images.
- Dose Computation: Time-integrated activity coefficients (TIACs) were calculated using bi-exponential fits, and OLINDA/EXM software was used to compute absorbed doses to organs-at-risk.
Future Directions in Personalized Cancer Treatment
The described dosimetry procedure offers a practical approach for routine clinical implementation, balancing accuracy with patient comfort. Results from this study align with findings from other research centers, reinforcing the reliability and applicability of the method.
By standardizing dosimetry procedures, researchers and clinicians can better understand the relationship between radiation dose and therapeutic outcomes, potentially leading to more individualized and effective treatments. Collaborative efforts to share and refine these techniques will further enhance the precision and safety of molecular radiotherapy.
As dosimetry methods become more refined and accessible, personalized cancer treatment strategies will become a reality, promising improved outcomes and reduced side effects for patients undergoing radionuclide therapy.
