Oral Hairy Leukoplakia: An Unexpected Early Warning Sign of Leukemia
"Could a tongue patch be more than just a harmless anomaly? Learn how oral hairy leukoplakia can sometimes signal a serious underlying condition."
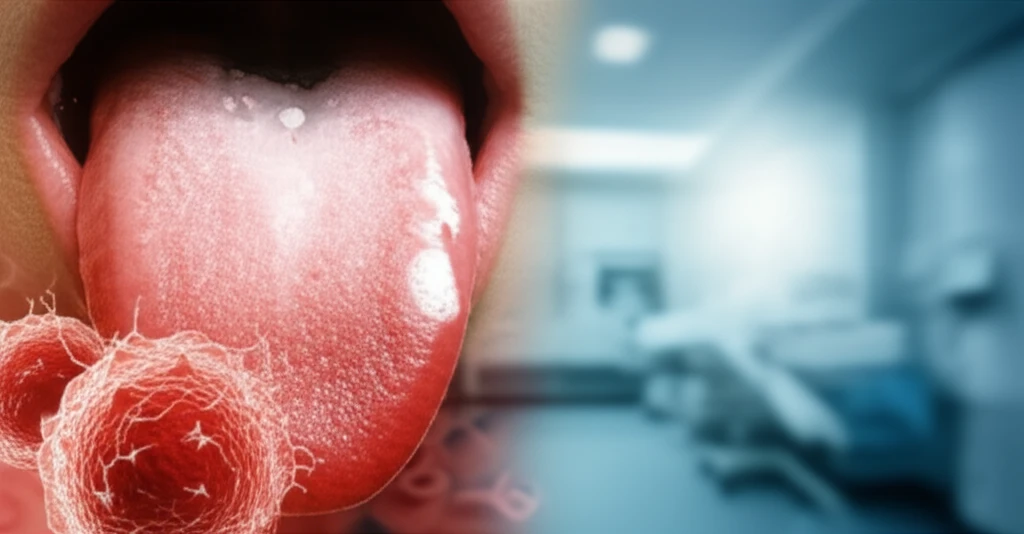
Oral hairy leukoplakia (OHL) is typically associated with the reactivation of the Epstein-Barr virus (EBV), manifesting as distinctive whitish patches, often corrugated or hairy in appearance, primarily on the sides of the tongue. While commonly linked to individuals with compromised immune systems, such as those with AIDS, OHL can also occur in other immunocompromised conditions.
In patients with leukemia, the occurrence of OHL is infrequent and typically arises following chemotherapy treatments. This article highlights a unique instance of OHL serving as the initial sign of acute myeloid leukemia (AML) in a previously healthy 15-year-old child, emphasizing the importance of recognizing such atypical presentations.
This article aims to raise awareness among both the public and healthcare professionals about the potential for OHL to indicate serious underlying conditions, even in the absence of typical risk factors. Early detection can significantly impact treatment outcomes and overall prognosis.
The Case: When a Tongue Patch Signaled Leukemia
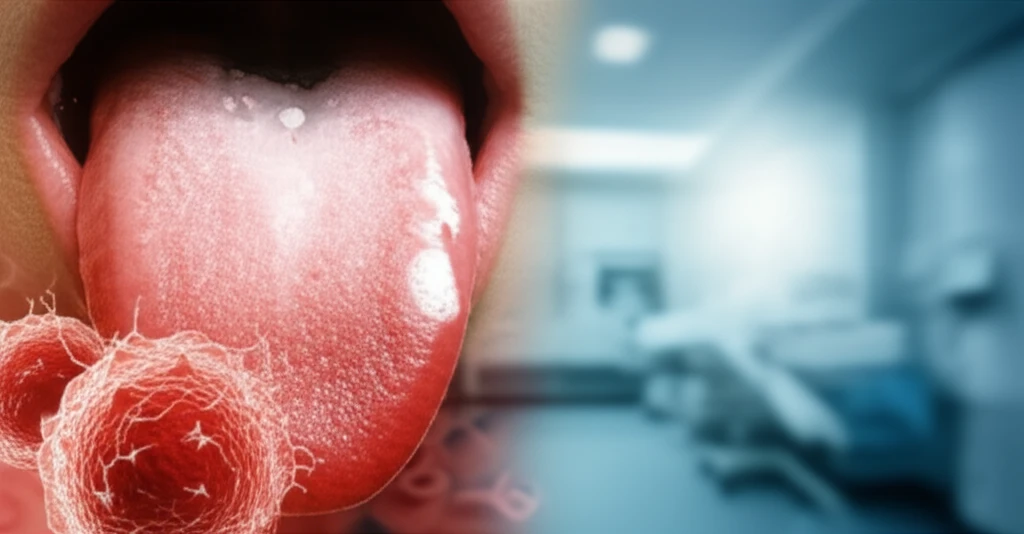
A 15-year-old boy, a soccer player with no prior medical issues, noticed a persistent whitish patch on the left side of his tongue. Initially asymptomatic, the lesion gradually increased in size, prompting medical evaluation. A physical examination revealed corrugated, firmly attached whitish patches that couldn't be easily scraped off.
- Papillomatosis (wart-like growths)
- Hyperkeratosis (thickening of the outer layer of skin)
- Parakeratosis (abnormal keratinization)
- Acanthosis (thickening of the prickle cell layer)
- Ballooning degeneration in the stratum spinosum (a specific layer of the epidermis)
Why This Case Matters: Recognizing the Unexpected
While OHL is commonly associated with immunosuppression, this case underscores the rare possibility of it being an initial sign of acute myeloid leukemia. Recognizing such atypical presentations is crucial for early diagnosis and intervention.
This case emphasizes the importance of thorough medical evaluation when encountering unusual oral lesions, especially in individuals without apparent risk factors for immunosuppression. Though rare, considering the possibility of underlying systemic diseases like leukemia can significantly impact patient outcomes.
Although OHL is not generally considered a prognostic indicator except in AIDS, this instance suggests that, when associated with hematologic malignancies, it might indicate an advanced stage or poorer prognosis. This highlights the need for further research to understand the relationship between OHL and leukemia outcomes.
