Nose-to-Brain Drug Delivery: Revolutionizing Treatment with Nanotechnology
"Explore how nanoparticles are bypassing the blood-brain barrier to deliver drugs directly to the brain via nasal administration, offering new hope for neurological disorders."
The pharmaceutical industry is increasingly focused on addressing unmet medical needs, leading to the development of innovative drugs with significant therapeutic impact. While advancements have been made in treating conditions like age-related macular degeneration and certain cancers, neurological disorders such as brain tumors, Alzheimer's disease, and Parkinson's disease remain challenging due to the difficulty of delivering drugs effectively to the brain.
A major hurdle in treating brain disorders is the blood-brain barrier (BBB), a protective mechanism that restricts the passage of most drugs from the bloodstream into the brain. This barrier prevents many potentially therapeutic compounds from reaching their targets in the brain, limiting treatment options for neurological conditions.
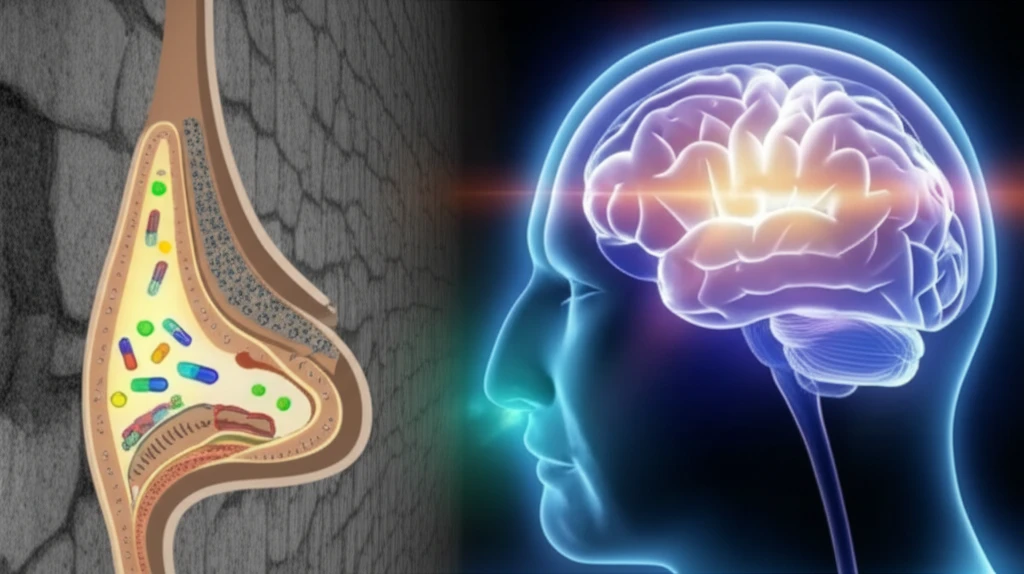
To overcome the BBB, researchers are exploring alternative drug delivery methods, with intranasal administration emerging as a promising non-invasive approach. This method allows drugs to bypass the BBB and directly target the brain, offering new possibilities for treating neurological disorders. This article will delve into the innovative use of nanoparticles for intranasal drug delivery, focusing on their ability to enhance drug transport and therapeutic efficacy in the brain.
Nanoparticles: A Key to Bypassing the Blood-Brain Barrier
Nanoparticles, such as liposomes and polymeric micelles, have emerged as versatile drug carriers, capable of encapsulating drugs and targeting specific tissues. These nanoparticles can be modified to enhance their stability, prolong their circulation in the bloodstream, and improve their ability to cross biological barriers like the BBB. Their unique properties make them ideal candidates for intranasal drug delivery to the brain.
- Enhanced Drug Encapsulation: They efficiently encapsulate drugs for targeted delivery.
- Improved Stability: They protect drugs from degradation, ensuring they reach their target.
- Biocompatibility: They are made from biocompatible materials, minimizing toxicity.
- Tunable Size: The size of micelles can be adjusted to optimize drug delivery.
The Future of Brain Disorder Treatment
The use of nanoparticles for intranasal drug delivery represents a significant advancement in the treatment of neurological disorders. By bypassing the blood-brain barrier and delivering drugs directly to the brain, these innovative approaches offer new hope for patients with conditions that were previously difficult to treat.
While challenges remain, ongoing research is focused on optimizing nanoparticle design, improving drug encapsulation and release, and enhancing targeting strategies. As these technologies continue to evolve, they hold the potential to revolutionize the treatment of brain tumors, Alzheimer's disease, Parkinson's disease, and other debilitating neurological conditions.
With further development and clinical validation, intranasal nanoparticle drug delivery could become a mainstream approach for treating a wide range of brain disorders, offering improved outcomes and a better quality of life for patients and their families. The future of brain disorder treatment is bright, with nanotechnology leading the way.
