Joint Relief Revolution: Can MSC-Exosomes and TGF-β1 Be the Future of Osteoarthritis Treatment?
"Unlocking the potential of MSC-exosomes and TGF-β1 in regulating chondrocyte proliferation for groundbreaking osteoarthritis therapies."
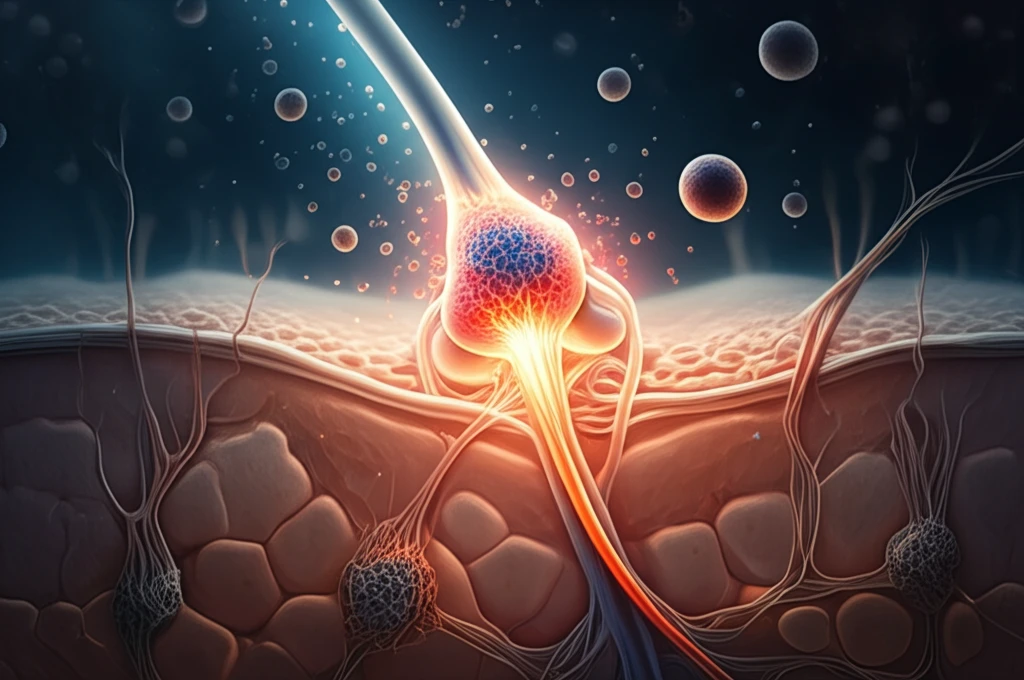
Osteoarthritis (OA), a widespread chronic joint condition, is characterized by the deterioration of articular cartilage, significantly impacting mobility and quality of life. Current treatments primarily focus on alleviating pain, but lack the ability to repair or regenerate damaged cartilage. The exploration of innovative therapeutic approaches is crucial to address this gap and provide more effective long-term solutions for OA patients.
Mesenchymal stem cells (MSCs) have emerged as promising candidates in regenerative medicine due to their capacity to modulate immune responses, stimulate tissue repair, and secrete exosomes—nanoscale vesicles containing proteins, RNAs, and other bioactive molecules. MSC-derived exosomes have demonstrated potential in promoting cartilage repair by encouraging chondrocyte proliferation and preventing apoptosis, making them a focal point in OA research.
Transforming growth factor-β1 (TGF-β1), a potent cytokine, plays a crucial role in cartilage repair and maintenance. Studies suggest that TGF-β1 enhances the therapeutic effects of MSC-exosomes, offering a synergistic approach to treating OA. However, the precise mechanisms by which TGF-β1 influences MSC-exosome-mediated cartilage repair remain an area of active investigation.
How Does TGF-β1 Boost Cartilage Repair Through MSC-Exosomes?
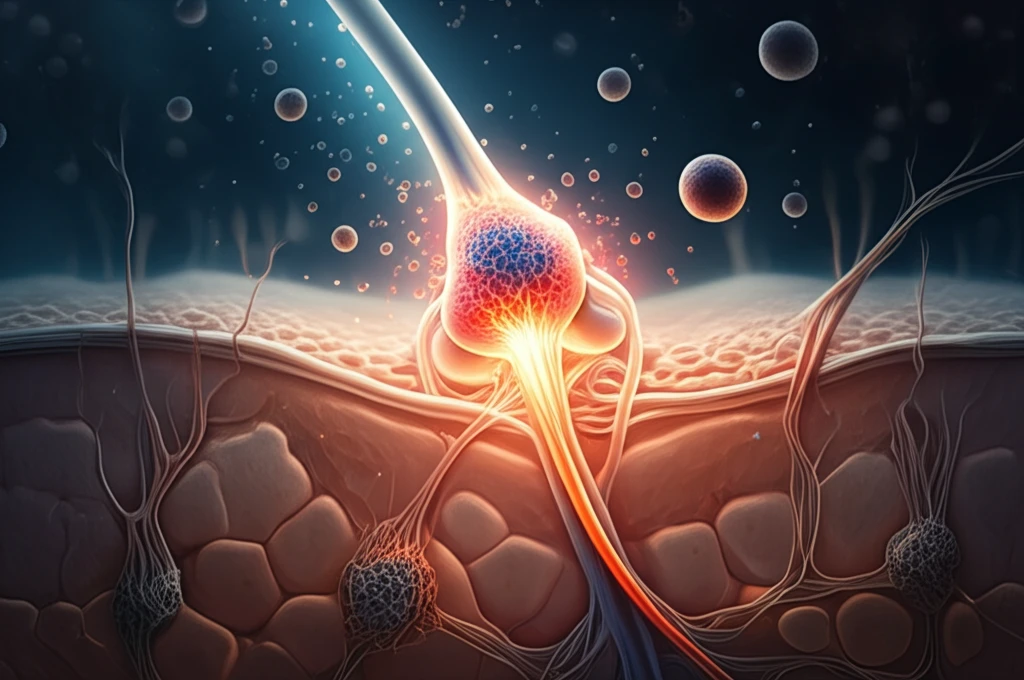
A recent study shed light on the intricate relationship between TGF-β1, MSC-exosomes, and chondrocyte proliferation. The researchers aimed to uncover the molecular mechanisms through which TGF-β1 regulates chondrocyte behavior via MSC-exosomes. By employing an experimental rat model of OA, they investigated the impact of TGF-β1 on MSC-exosome composition and its subsequent effects on cartilage repair.
- Establishing an OA rat model to mimic the disease environment.
- Stimulating MSCs with TGF-β1 to observe changes in exosome composition.
- Analyzing the expression of miR-135b and Sp1 in MSCs, MSC-exosomes, and chondrocytes.
- Assessing chondrocyte viability using MTT assays to measure cellular metabolic activity.
The Future of Joint Care: What Does This Mean for You?
This research highlights the potential of MSC-exosomes and TGF-β1 as therapeutic agents for osteoarthritis. By understanding the molecular mechanisms involved in cartilage repair, scientists are paving the way for innovative treatments that could alleviate pain, restore joint function, and improve the quality of life for millions affected by OA. Although further studies are needed to translate these findings into clinical applications, the future of joint care looks promising.
