IVT vs. Direct MT: Decoding the Best Stroke Treatment Strategy
"Is combining IVT with mechanical thrombectomy the gold standard, or is direct MT a better approach? The debate continues as new research sheds light on optimal stroke care."
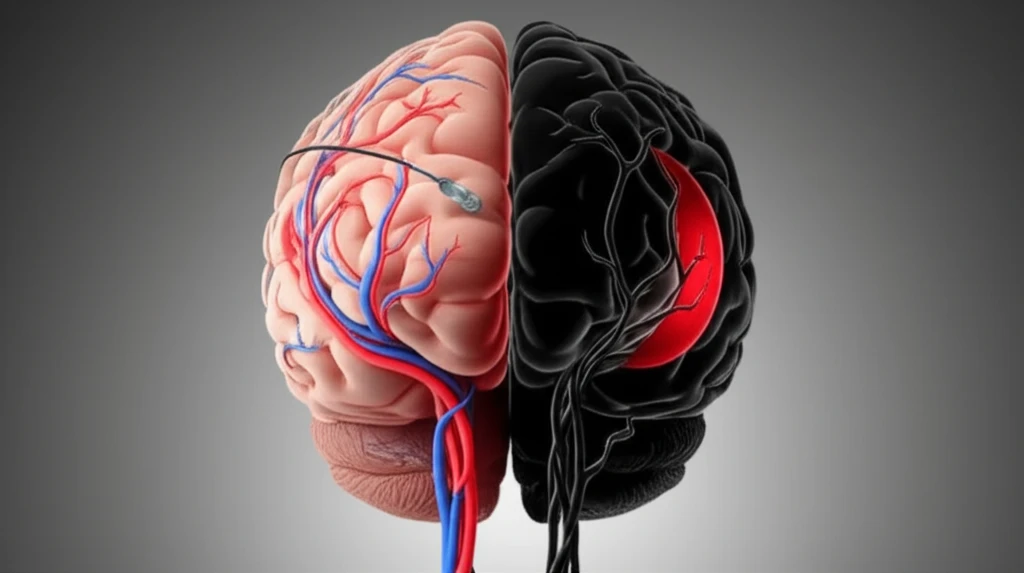
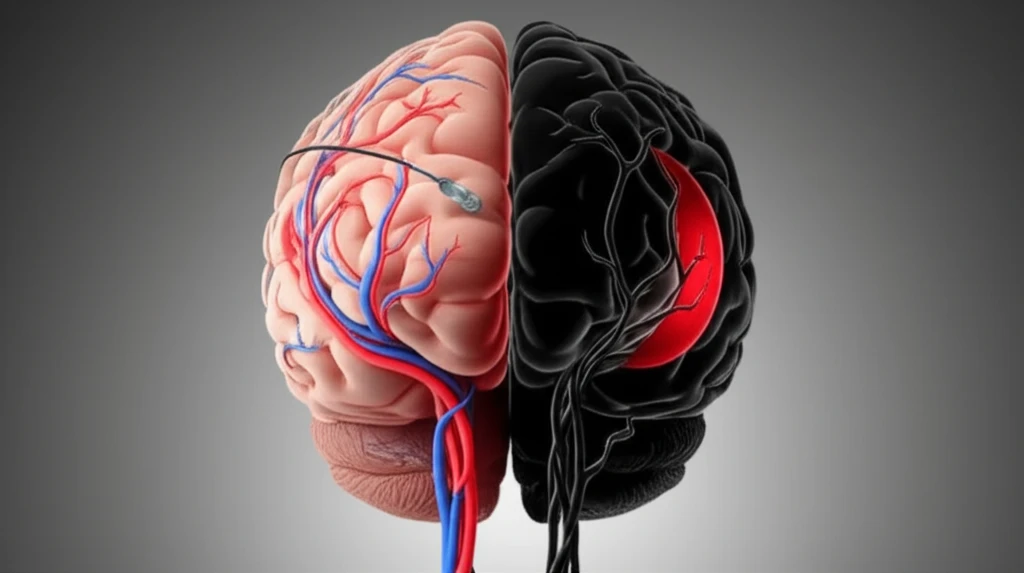
Stroke, a leading cause of long-term disability, demands swift and effective intervention. For large vessel occlusions (LVOs), the treatment landscape has evolved, presenting two primary strategies: intravenous thrombolysis (IVT) followed by mechanical thrombectomy (MT), or direct mechanical thrombectomy (dMT) alone. The question of which approach yields superior outcomes remains a subject of intense debate and ongoing research.
Intravenous thrombolysis (IVT), often referred to as 'clot-busting' medication, has long been a cornerstone of acute stroke treatment. However, its effectiveness in dissolving large clots, particularly in major cerebral arteries, can be limited. Mechanical thrombectomy (MT) offers a more direct approach, physically removing the clot using specialized devices. The combination of IVT and MT aims to leverage the benefits of both techniques, but whether this combined approach truly outperforms dMT is a critical question.
Recent studies, including the one by Goyal et al., have fueled this debate. While some findings suggest that IVT prior to MT is associated with better functional outcomes, other researchers emphasize the need to account for confounding factors such as blood pressure and pre-existing coagulopathies. This article delves into the nuances of these arguments, exploring the evidence and expert opinions shaping the future of stroke treatment.
IVT Before MT: Does It Really Make a Difference?
Goyal et al.'s multicenter observational study, titled “Comparative safety and efficacy of combined IVT and MT with direct MT in large vessel occlusion,” sparked considerable discussion. Their findings indicated that IVT before MT was linked to a higher likelihood of functional independence three months post-stroke. This suggests that IVT may play a crucial role in improving long-term outcomes for stroke patients with LVOs.
- Reduced Infarction Risk: IVT may protect against new infarcts in previously healthy brain tissue.
- Improved Recanalization Chances: IVT can improve the chances of successful blood flow restoration, especially when thrombectomy alone is insufficient.
- Functional Independence: Studies suggest a link between IVT before MT and improved long-term functional outcomes.
The Road Ahead: Waiting for Definitive Answers
The optimal stroke treatment strategy for LVOs remains a complex and evolving area. While existing evidence provides valuable insights, the limitations of observational studies necessitate caution in drawing firm conclusions. As ongoing prospective clinical trials, such as MR CLEAN-NO IV and SWIFT DIRECT, release their findings, a clearer picture will emerge regarding the true superiority of combined IVT and MT versus MT alone. Until then, clinicians must weigh the available evidence, consider individual patient factors, and adhere to established guidelines to deliver the best possible care.
