Dialysis Access Revolution: How New Graft Tech Could Change Lives
"Prosthetic grafts are a lifeline for hemodialysis patients, but improving their patency is crucial. Discover the innovative strategies and future tech aiming to extend the life of these vital vascular accesses."
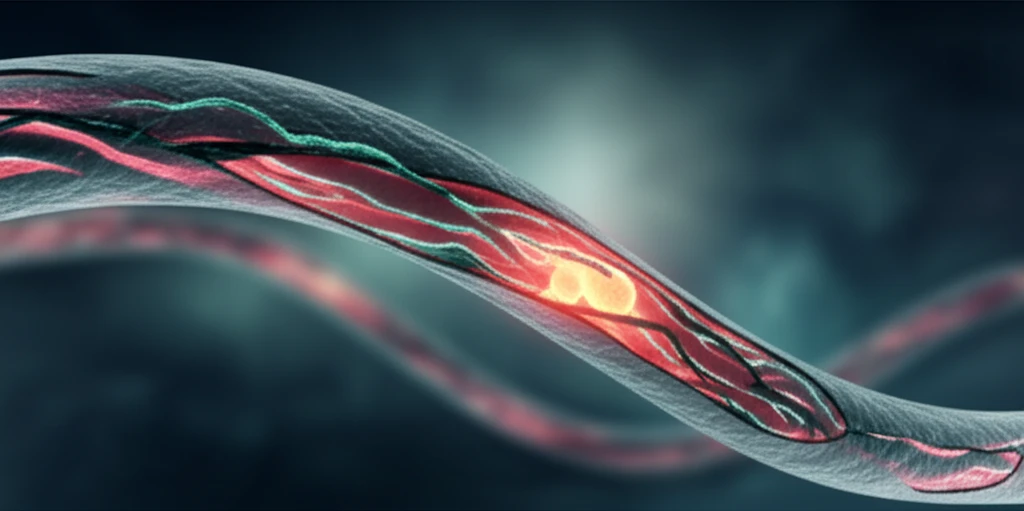
For individuals with end-stage renal disease, hemodialysis is a critical procedure. As the population requiring dialysis grows, particularly among the elderly and those with diabetes, the need for reliable vascular access becomes increasingly important. When arteriovenous fistulas (AVFs) – the preferred access method – aren't feasible, prosthetic arteriovenous grafts (AVGs) become essential.
However, AVGs have a significant drawback: they don't last as long as AVFs. These grafts often develop problems like neointimal hyperplasia (NIH), a thickening of the vessel lining that leads to narrowing and eventual failure. This means more procedures, more costs, and more disruption for patients.
The focus has shifted to innovative ways to enhance AVGs and materials. This article explores the latest strategies in graft modification, from altering the physical design to incorporating advanced drug coatings and surface technologies, all aimed at improving AVG patency and, ultimately, patient outcomes.
Can Geometry and Smarter Design Extend Graft Lifespan?
Researchers are exploring how altering the shape and structure of AVGs can optimize blood flow and reduce the risk of complications. The goal is to create a more natural, laminar flow, minimizing turbulence and areas of high or oscillating wall shear stress (WSS), which are known to contribute to NIH.
- The Venaflo™ Graft: Features a cuff at the venous end designed to reduce WSS. While early studies showed promise, issues with pseudo-intima formation within the cuff limited its overall effectiveness.
- The Bi-Flow Graft: An evolution of the Venaflo, this graft uses a diffuser with two flow channels to further minimize WSS and flow separation. Animal studies are needed to confirm its potential.
- Tapered Grafts: These grafts increase resistance at the artery connection, reducing flow and WSS within the graft. However, high resistance may cause hemolysis. Clinical results have been mixed, highlighting the need for optimized tapering methods.
- Helical Grafts: Mimicking the natural spiral shape of arteries, these grafts aim to create a more natural, laminar flow. Early clinical results were not promising, as the helical structure tended to diminish after implantation. Solutions like the C-flex connector are being explored.
The Future of AVGs: A Path to Longer-Lasting Access
While modifying flow hemodynamics shows theoretical promise, clinical results have been inconsistent. Issues such as the lack of a functional endothelial lining on grafts remain a significant challenge. This natural lining provides crucial benefits like reducing thrombogenicity and NIH formation.
Exciting advancements are focusing on creating this endothelial lining through surface modifications. Plasma treatment and nanotopography are being explored to enhance the hydrophilic properties of graft surfaces and promote endothelial cell adhesion. Electrospun grafts, like the AVflo™, are designed to encourage graft maturation and early cannulation.
Ultimately, the future of AVGs lies in combining these approaches: optimizing graft design for better hemodynamics, incorporating drug coatings to prevent NIH and thrombosis, and engineering graft surfaces to promote endothelialization. These advancements promise to significantly improve the lives of hemodialysis patients by providing longer-lasting, more reliable vascular access.
