Decoding Pancreatic Cancer: How Precise Margin Assessment Can Improve Outcomes
"A deep dive into how color-coded tissue marking enhances the accuracy of surgical margin evaluation and its impact on recurrence-free survival for pancreatic cancer patients."
Pancreatic cancer, particularly pancreatic ductal adenocarcinoma (PDAC), remains one of the most aggressive and challenging cancers to treat. Despite advancements in detection and treatment, the overall five-year survival rate hovers around a discouraging 6%. Surgical resection, specifically pancreatoduodenectomy, offers the best chance for a cure, yet only a small fraction of patients are eligible due to the advanced stage of the disease at diagnosis. For those who undergo surgery, achieving negative surgical margins—where no cancer cells are present at the edge of the removed tissue—is critical for improving prognosis.
However, determining what constitutes an adequate surgical margin has been a subject of ongoing debate. The complex anatomy of the pancreas, coupled with variable tumor characteristics, makes it difficult to standardize the evaluation of surgical margins. Traditional methods often rely on macroscopic evaluation and sampling from representative areas, which may not capture the full extent of tumor involvement. This lack of standardization has led to conflicting results in studies examining the impact of surgical margins on patient survival.
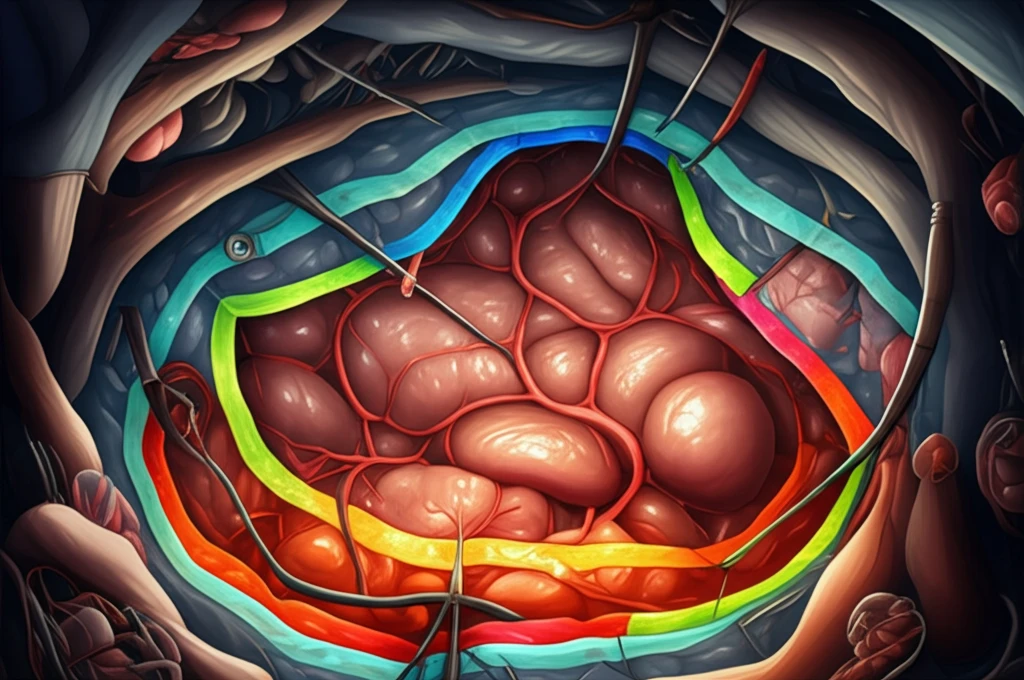
A recent study published in "Pancreas" journal sheds light on this critical issue by employing a color-coding method with tissue marking dyes to meticulously evaluate surgical margins. This innovative approach aims to provide a more accurate assessment of margin status and its correlation with postoperative recurrence, offering new insights into optimizing surgical strategies for pancreatic cancer.
The Color-Coding Revolution in Surgical Margin Assessment
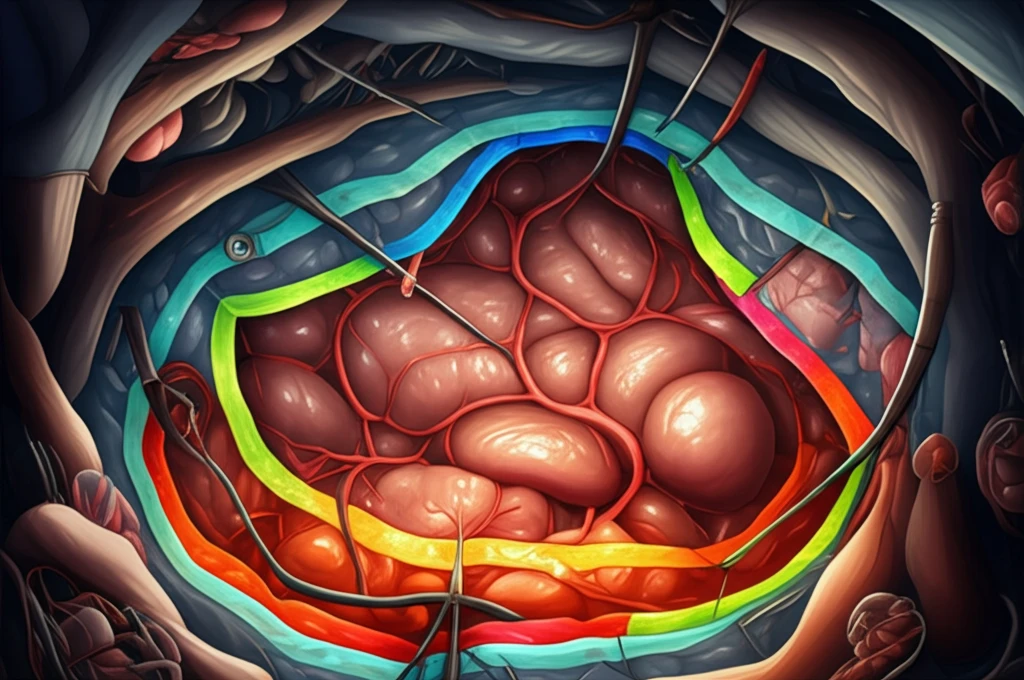
The cornerstone of this study is the implementation of a unified protocol for processing pancreatoduodenectomy specimens. This protocol involves marking five surgical margins with distinct colors using tissue-marking dyes. These margins include the anterior surface, posterior margin, portal vein/superior mesenteric vein (PV/SMV) groove margin, superior mesenteric artery (SMA) margin, and the pancreas cut-end margin (PCM). This color-coding technique allows pathologists to systematically evaluate each margin and precisely measure the resection margin distance (RMD)—the distance from the closest tumor cell to the marked margin.
- Improved Standardization: Provides a consistent method for margin assessment.
- Enhanced Accuracy: Allows for precise measurement of resection margin distance.
- Better Risk Stratification: Helps identify patients at higher risk of locoregional recurrence.
- Potential for Personalized Treatment: May inform decisions about adjuvant therapy.
A Path Forward in Pancreatic Cancer Treatment
This study underscores the critical role of precise surgical margin assessment in improving outcomes for pancreatic cancer patients. The color-coding method offers a standardized, accurate approach that can help surgeons and pathologists better evaluate resection margins and identify patients at high risk for recurrence. While early detection of small-sized tumors without lymph node metastasis remains paramount, optimizing surgical techniques and margin assessment is a crucial step towards enhancing the effectiveness of pancreatic cancer treatment and improving patient survival rates. Further research is needed to validate these findings and explore the potential for personalized treatment strategies based on margin status. As we continue to refine our approaches, the hope for better outcomes in this challenging disease grows ever stronger.
