Decoding ECGs: Why 12-Lead is the Gold Standard
"Understanding the importance of comprehensive electrocardiograms for accurate cardiac diagnosis."
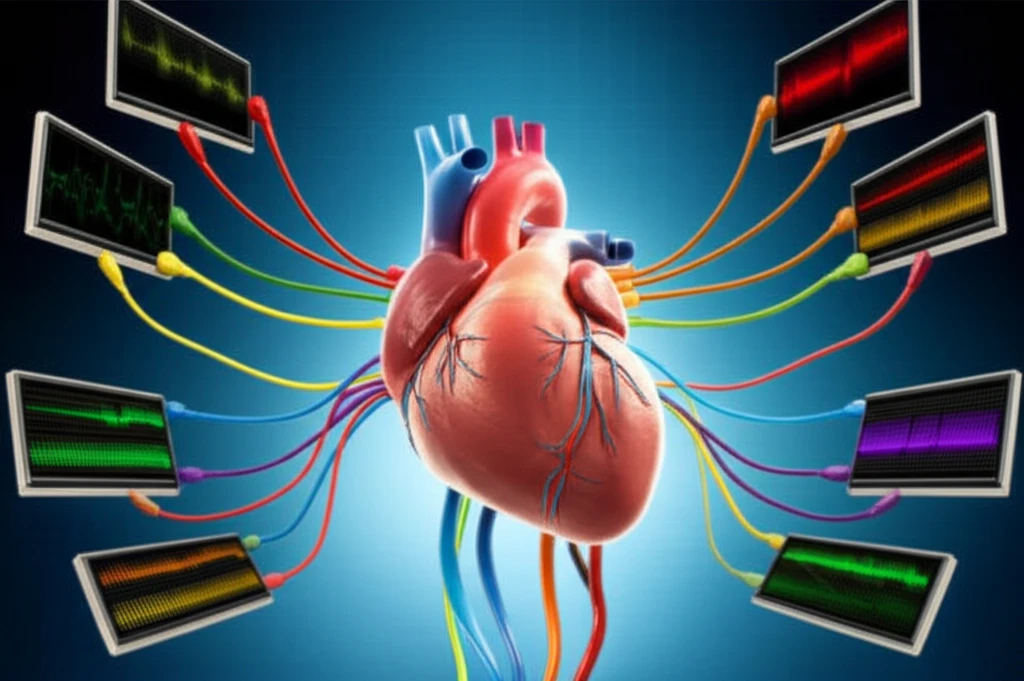
Electrocardiograms (ECGs) are a cornerstone of cardiac care, providing a snapshot of the heart's electrical activity. While quick rhythm strips can offer some insight, they often fall short in providing a complete picture.
A recent case highlighted the critical difference between a limited ECG and a comprehensive 12-lead ECG. A student nurse initially recorded a routine ECG using a 3-lead rhythm strip, which appeared to indicate a dangerous ventricular standstill.
However, a subsequent 12-lead ECG revealed a much different story: a sinus rhythm with premature ventricular contractions. This stark contrast underscores the importance of using the right tool for accurate diagnosis and patient care.
The Superiority of 12-Lead ECGs: Seeing the Full Picture
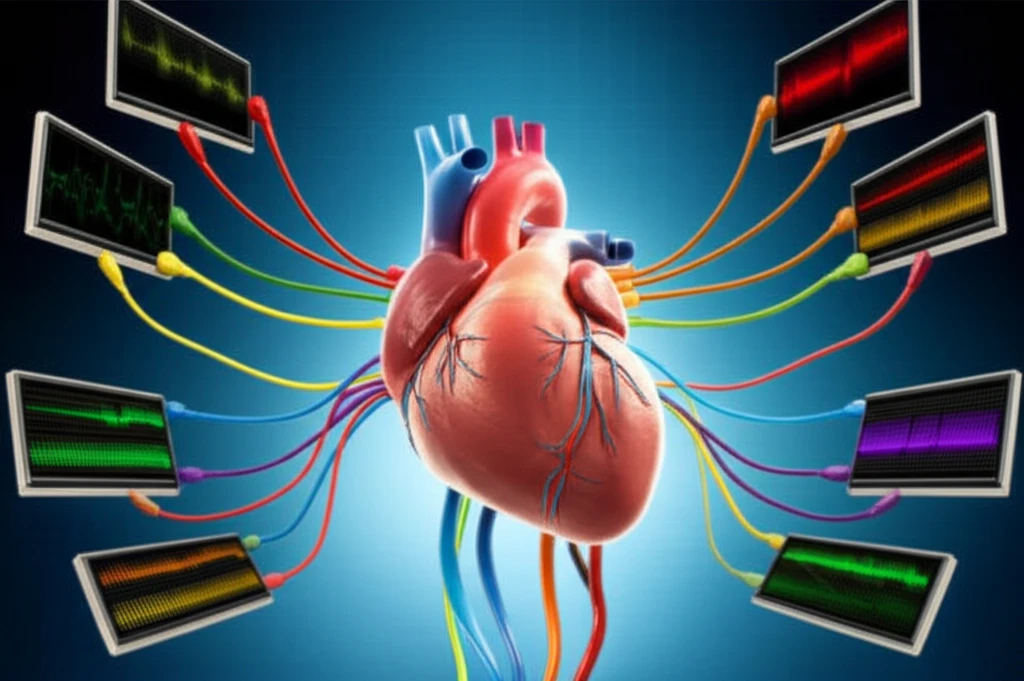
A 12-lead ECG provides a more detailed view of the heart's electrical activity from multiple angles. This comprehensive approach allows clinicians to:
- Detect subtle abnormalities: Identify issues that may be missed by simpler ECG methods.
- Pinpoint the location of damage: Determine the specific areas of the heart affected by ischemia or infarction.
- Differentiate between conditions: Distinguish between various arrhythmias and other cardiac abnormalities.
- Guide treatment decisions: Provide a more accurate basis for developing effective treatment plans.
Postoperative Bleeding Management: A Proactive Approach
Beyond accurate diagnostics, proactive management of potential complications is crucial. Postoperative bleeding, as highlighted by Laider S (2012), is a significant concern in cardiac surgery.
Coakley et al (2011) emphasized the importance of early identification of patients at risk for bleeding. A comprehensive preoperative assessment, including detailed family history, is essential to identify potential bleeding risks.
By implementing checklists and ensuring staff competency in assessing and managing bleeding risks, healthcare providers can significantly improve patient outcomes and maintain a high standard of care.
