Decoding Drug Resistance: How New Technologies are Personalizing Antibiotic Treatment
"The battle against superbugs takes a personalized turn as advanced diagnostic tools promise to tailor antibiotic prescriptions for individual patients, optimizing treatment and slowing the spread of resistance."
For decades, antimicrobial agents have been the cornerstone of treating severe microbial infections. While dosage strategies, administration routes, and innovative drug combinations are critical, the increasing adaptability of microbes often leads to treatment failures and the rise of antibiotic resistance. This is leaving medical professionals in search of more effective ways to combat infections.
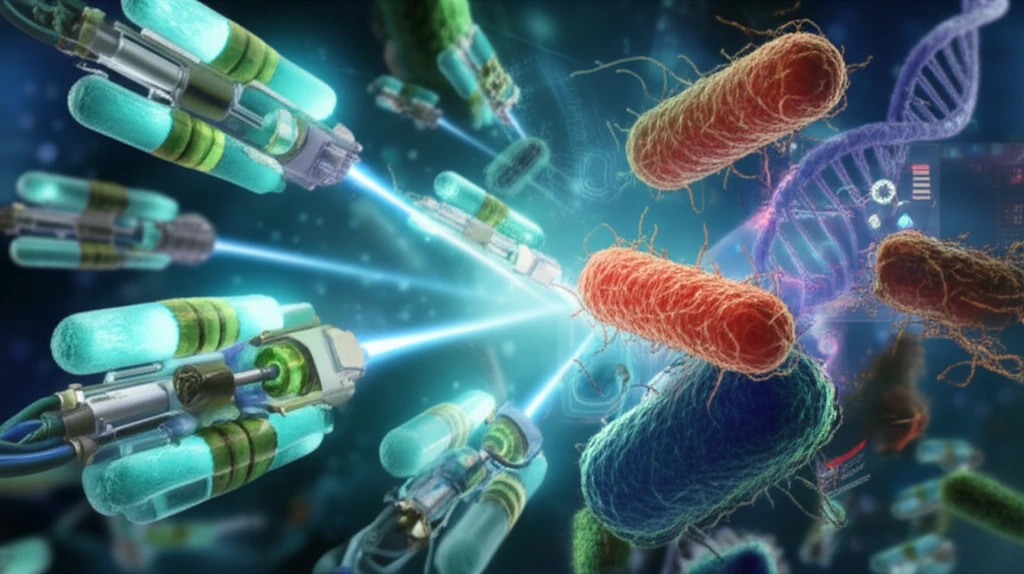
As our arsenal of effective antibiotics dwindles, understanding and predicting resistance mechanisms become crucial. Bacteria are incredibly versatile, developing resistance through various means, from protecting themselves within heterogeneous populations to acquiring resistance genes. This demands newer agents and a better understanding of how to use existing ones.
This article explores how in vitro antimicrobial susceptibility testing (AST) is evolving to meet these challenges. By assessing how bacteria respond to antibiotics, AST helps guide treatment decisions and track resistance trends. We'll delve into the latest advancements, including automated systems and genomic methods, that promise to personalize antibiotic therapy and improve patient outcomes.
The Evolving Landscape of Antibiotic Susceptibility Testing
AST traditionally measures the minimum inhibitory concentration (MIC) and minimum bactericidal concentration (MBC) of antibiotics, categorizing bacteria as resistant, intermediate, or susceptible. These tests quantify bacterial survival or death when exposed to different antibiotic concentrations.
- Automated Systems: Systems like VITEK 2, BD Phoenix, and MicroScan WalkAway automate the testing process, providing faster results and updated antimicrobial coverage.
- Disk Diffusion Automation: Systems are automating the interpretation of disk diffusion tests, reducing human error and optimizing microscopy readings.
- Emerging Technologies: Innovative methods focus on detecting resistance by measuring enzyme activity, identifying entities that block antibiotics, detecting resistance factors, analyzing intracellular changes, or assessing cellular expression changes.
A Future of Targeted Antibiotic Therapy
Current AST methods have limitations, particularly in the face of emerging pathogens and resistance traits. As Carl Nathan and Otto Cars noted in the New England Journal of Medicine, better diagnostic technology will allow for narrowly tailored antibiotic prescriptions, specifically targeting the pathogens' susceptibility.
The integration of advanced diagnostic tools into clinical practice promises to revolutionize infectious disease management. By providing rapid, accurate, and personalized insights into antibiotic resistance, these technologies will empower clinicians to optimize treatment strategies, minimize the spread of resistance, and improve patient outcomes.
With ongoing research and collaboration between academia, industry, and regulatory bodies, the future of AST is bright. As we move towards more sophisticated and individualized approaches, we can expect significant advancements in the fight against drug-resistant infections.
