Clearing the Air: Understanding Pulmonary Alveolar Proteinosis and the Role of Blood Testing
"Navigating the complexities of diagnosing PAP: Why blood tests may soon offer a less invasive path to clarity."
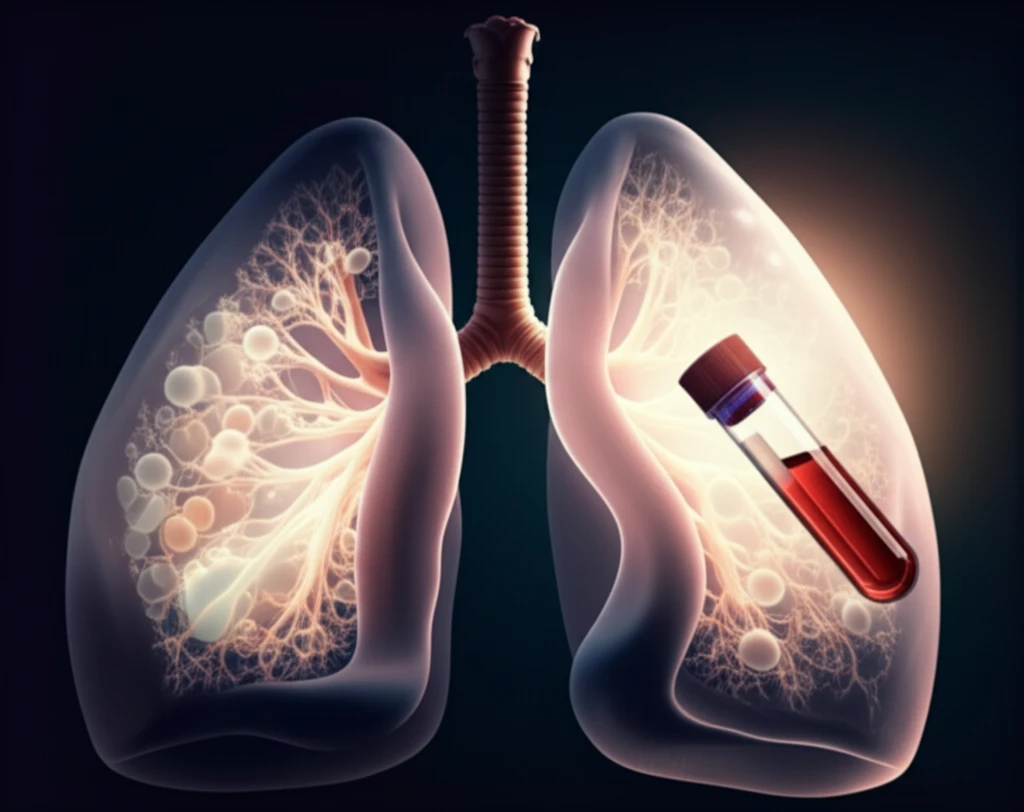
Pulmonary Alveolar Proteinosis (PAP) is a rare lung disorder characterized by the accumulation of surfactant in the alveoli, the tiny air sacs in the lungs. This build-up impairs gas exchange, leading to shortness of breath and other respiratory symptoms. Diagnosing PAP can be challenging, often requiring invasive procedures.
Traditionally, the diagnostic pathway involves a combination of clinical assessments, radiological imaging (such as CT scans), and bronchoscopy with bronchoalveolar lavage (BAL). BAL involves washing the lungs with fluid to collect samples for analysis, and sometimes a transbronchial biopsy is performed. While effective, these methods carry risks and may not be suitable for all patients.
In a recent exchange published in The Lancet Respiratory Medicine, researchers discussed the potential of using blood tests, specifically the detection of granulocyte-macrophage colony-stimulating factor (GM-CSF) autoantibodies, as a less invasive diagnostic tool for PAP. This article breaks down the key points of this discussion and explores what the future may hold for PAP diagnosis.
The Promise of GM-CSF Autoantibody Testing: A New Hope for PAP Diagnosis?
GM-CSF is a cytokine that plays a crucial role in the clearance of surfactant from the alveoli. In autoimmune PAP, the body produces autoantibodies against GM-CSF, impairing its function and leading to surfactant accumulation. Detecting these autoantibodies in the blood could offer a simpler, less invasive way to diagnose PAP.
- Sensitivity and Specificity: While GM-CSF autoantibodies are highly prevalent in autoimmune PAP (responsible for about 90% of cases), a negative result doesn't rule out other forms of PAP, such as secondary, congenital, or unclassifiable PAP.
- Availability and Standardization: GM-CSF autoantibody testing is not widely available and is often limited to specialized centers or used as a research tool. The methodology and cut-off values also lack standardization, hindering widespread clinical application.
- Clinical Context is key: Relying solely on blood tests without considering clinical and radiological findings can be misleading. The radiological characteristics of PAP, such as ground-glass opacities seen on CT scans, while suggestive, are not definitive.
The Future of PAP Diagnosis: A Path Towards Non-Invasive Solutions
Despite the current limitations, the authors express optimism about the future role of GM-CSF autoantibody testing in PAP diagnosis. They envision a scenario where blood testing, combined with high-resolution CT imaging, can accurately identify PAP, reducing the need for invasive procedures. This approach would require further research to validate the accuracy of these combined methods against the pathological gold standard.
