Building Better Bones: Scientists' Revolutionary Approach to Healing Fractures
"New research explores innovative ways to repair bone injuries using advanced materials and cell-based therapies, offering hope for faster and more effective healing."
Bone fractures, whether from a minor fall or a serious accident, are a common health issue affecting people of all ages. While the body naturally heals these breaks, the process can be slow, painful, and sometimes incomplete. Now, scientists are pushing the boundaries of medical science to accelerate and improve bone healing, focusing on innovative methods that could revolutionize how we treat fractures.
At the forefront of this research is bone tissue engineering, a field that uses a combination of materials, cells, and engineering principles to create biological substitutes for damaged bone. The goal is to develop treatments that not only mend broken bones but also restore the natural function and structure of the bone tissue.
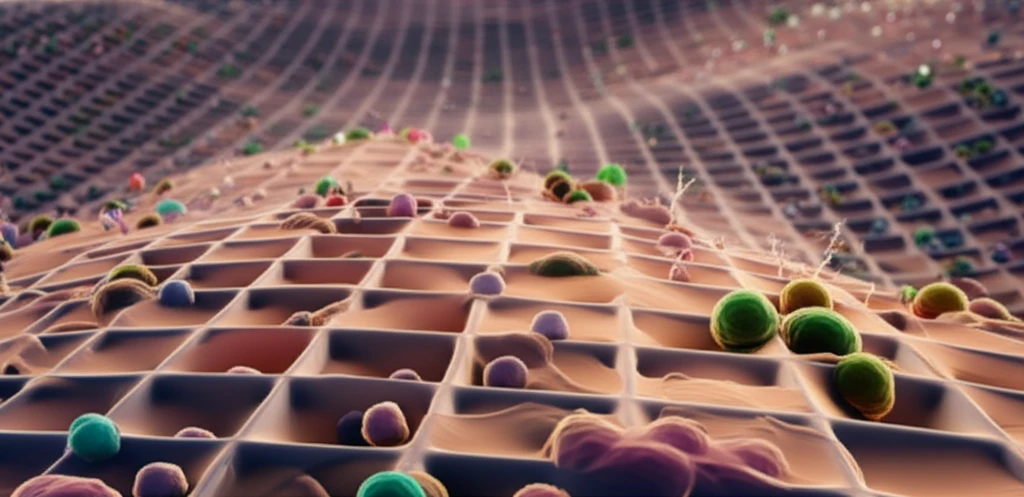
Recent studies have focused on enhancing the properties of 3D-printed scaffolds. These scaffolds, made from biocompatible materials, serve as a framework to support bone regeneration. One such study explores the use of surface modifications and RGD-immobilization to create a better environment for bone-forming cells to thrive.
The Science Behind the Breakthrough: Surface Modifications and Cell Behavior
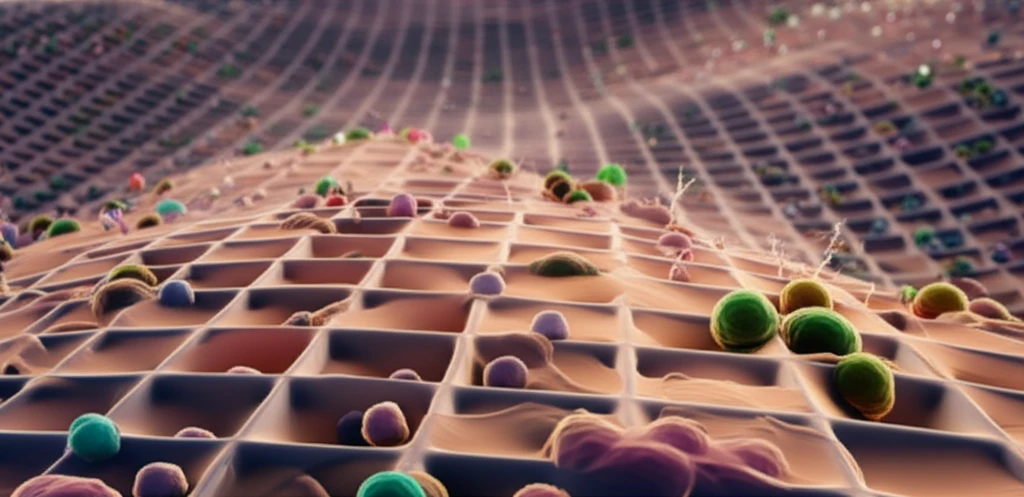
The research, published in 'Biomedical Materials', delves into the complex relationship between the surface properties of 3D-printed scaffolds and how they influence the behavior of bone-forming cells. Specifically, the study investigates the impact of modifying the surface of poly(ɛ-caprolactone) (PCL) scaffolds. PCL is a biocompatible polymer widely used in tissue engineering because of its ability to degrade naturally in the body. However, PCL on its own is not ideal for bone regeneration due to its hydrophobic nature and lack of cell-recognition sites.
- Surface modifications enhance cell attachment, proliferation, and differentiation.
- Chemical modifications using NaOH create a more hydrophilic environment.
- RGD-immobilization introduces cell-recognition sites.
The Future of Fracture Repair: Promising Avenues for Further Research
The research on surface-modified scaffolds represents a significant step forward in bone tissue engineering. By understanding how to manipulate the surface properties of these materials, scientists can create more effective frameworks for bone regeneration. The next steps for this research include further investigations into the long-term effects of these treatments and translating these findings into clinical applications. With continued research and innovation, the future of fracture repair looks promising, offering the potential for faster recovery and improved quality of life for individuals with bone injuries.
