Breathe Easier: A Modern Guide to Trachea and Bronchus Surgery
"Understanding anesthesia options and surgical techniques for a smoother recovery."
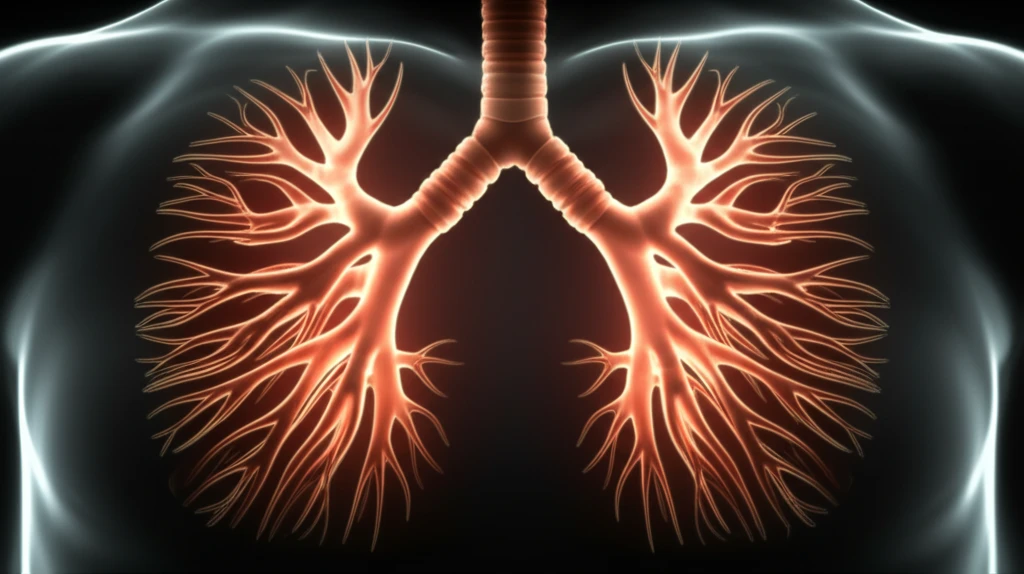
The central airway, encompassing the trachea, main stem bronchi, and lobar bronchi, is vital for breathing. When disorders strike this area, causing symptoms like cough, dyspnea, and stridor, surgery becomes a key treatment option. These surgeries, crucial for addressing conditions from stenosis to traumatic injuries and tumors, demand careful planning and execution.
Anesthesia plays a pivotal role in these procedures. Effective anesthesia management not only ensures patient comfort but also safeguards the integrity of the airway during surgery. Given the potential for higher mortality and morbidity rates associated with these surgeries, a collaborative approach between surgeons and anesthesiologists is essential.
This guide explores the latest advancements in anesthesia for tracheal and bronchial surgeries, highlighting techniques that enhance patient safety and improve surgical outcomes. We'll cover everything from pre-operative assessments to post-operative care, providing you with a comprehensive understanding of this complex field.
Navigating Tracheal Stenosis: From Diagnosis to Treatment
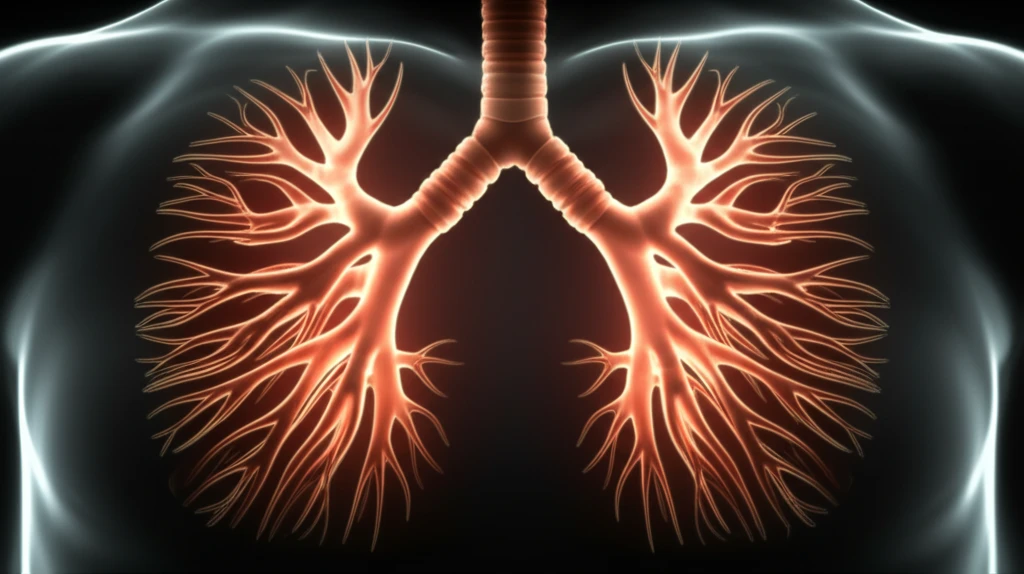
Tracheal stenosis, a common reason for trachea and bronchus surgery, arises from various factors, with post-intubation and post-tracheostomy being the most frequent causes. The condition, which narrows the trachea, can also stem from congenital diseases, inflammatory conditions, infections, or tumors. Recognizing the signs and understanding the underlying causes are the first steps toward effective management.
- Pulmonary Function Tests: Flow-volume loops can indicate the degree of stenosis.
- Imaging (CT/MRI): Provides detailed views of the trachea.
- Flexible Bronchoscopy: Allows direct visualization of the airway.
Looking Ahead: Innovations in Airway Surgery
The field of trachea and bronchus surgery is constantly evolving, with ongoing research and technological advancements paving the way for improved patient outcomes. From minimally invasive techniques to enhanced anesthesia protocols, the future holds promise for safer and more effective interventions.
Collaboration between surgeons, anesthesiologists, and other healthcare professionals remains at the heart of successful airway surgery. By staying informed and embracing new knowledge, medical teams can provide the best possible care for patients with tracheal and bronchial disorders.
Whether you're a patient, caregiver, or healthcare provider, understanding the latest developments in this field is essential. This guide provides a starting point for further exploration, empowering you to make informed decisions and advocate for optimal respiratory health.
