When Your Gut Takes a Detour: Understanding Thoracoabdominal Hernias
"A Rare Case Highlights the Importance of Recognizing Unusual Herniations"
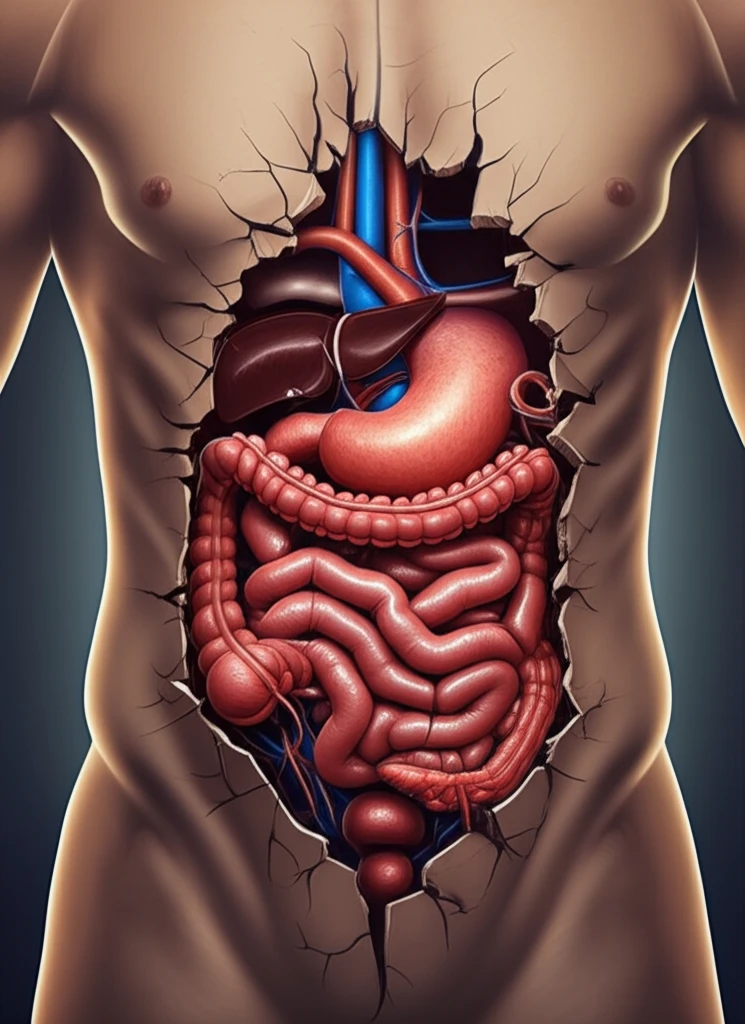
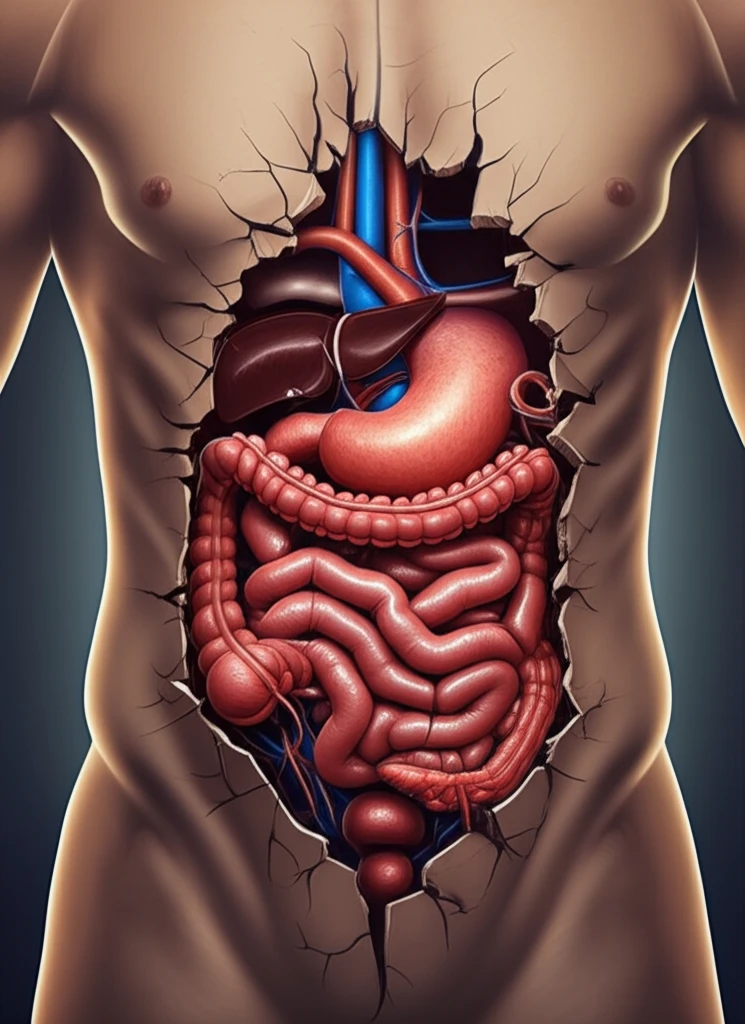
Imagine your body as a complex network of interconnected systems, each playing a vital role in maintaining overall health. Now, picture a scenario where one of these systems—your digestive tract—takes an unexpected detour, venturing into a space it doesn't normally occupy. This is essentially what happens in a thoracoabdominal hernia, a rare condition where abdominal organs, like the intestines, push through a defect and migrate into the chest cavity.
Thoracoabdominal hernias are uncommon occurrences, typically arising after significant blunt trauma. In these cases, a rupture in the diaphragm, the muscle separating the chest and abdomen, allows abdominal contents to herniate upwards into the thorax. However, not all hernias follow this conventional pathway. A recent case report details an atypical presentation of this condition, challenging our understanding and highlighting the importance of considering alternative routes of herniation.
This article will delve into a fascinating case of thoracoabdominal herniation that defied expectations. We'll explore the details of the patient's journey, from initial trauma to diagnosis and eventual surgical repair. By examining this unique scenario, we aim to shed light on the complexities of thoracoabdominal hernias and underscore the need for vigilance and tailored treatment approaches.
Atypical Herniation: Bypassing the Diaphragm
The case involves a 72-year-old woman with a history of hypertension, hypothyroidism, and asthma who sustained multiple injuries in a road traffic accident. Initial assessments revealed several right-sided issues, including fractures and a haemopneumothorax. Notably, she was also diagnosed with a traumatic hernia involving the hepatic flexure of the colon, protruding through the anterolateral abdominal wall.
- Passed through the transversus abdominis and internal oblique muscles.
- Traveled cranially between the internal and external oblique muscles.
- Entered the thoracic cavity through a defect in the thoracic wall.
- Completely bypassed the diaphragm.
The Importance of Vigilance and Definitive Repair
This unique case underscores the importance of maintaining a high index of suspicion for thoracoabdominal herniation in patients presenting with respiratory or gastrointestinal symptoms following trauma. While imaging plays a crucial role in guiding management, clinicians must be aware of its limitations and the potential for atypical presentations. Early and definitive surgical repair remains the cornerstone of treatment, aiming to restore anatomical integrity and prevent potentially life-threatening complications.
