When a Biliary Stent Goes Rogue: Understanding and Preventing Migration Complications
"A rare but serious case highlights the risks of biliary stent migration and the importance of vigilant post-procedure monitoring."
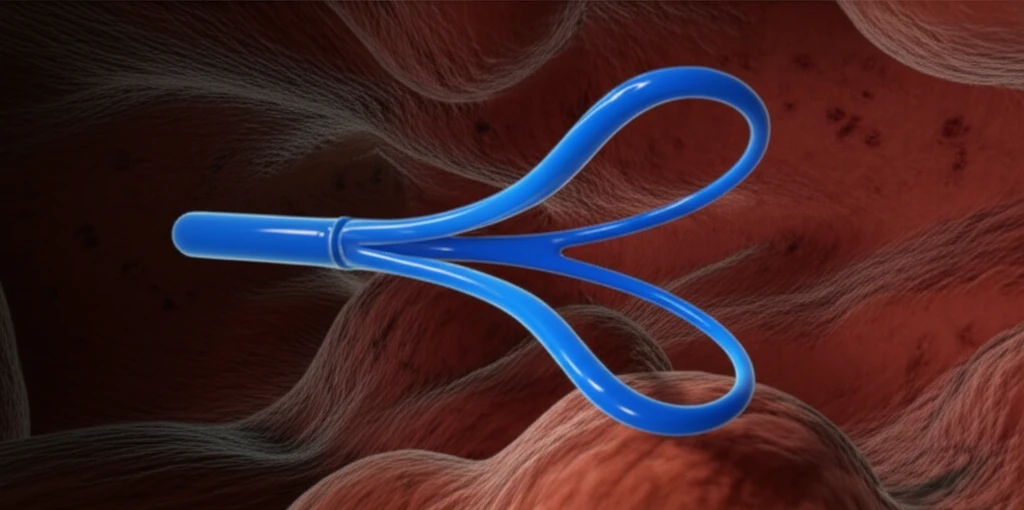
Biliary stents are essential tools in modern medicine, designed to widen bile ducts narrowed by malignant or benign conditions. These small tubes, typically placed endoscopically, help ensure proper bile flow and alleviate obstructive symptoms. While biliary stent placement is a routine procedure, it's not without risks. Complications can range from mild to severe, impacting patient health and requiring further intervention.
One of the more unusual but serious complications is stent migration, where the device moves from its intended location. In rare instances, this migration can lead to intestinal perforation, a life-threatening condition requiring immediate surgical attention. Understanding the risk factors, preventative measures, and recognition of atypical symptoms are crucial for healthcare providers and patients alike.
This article delves into a case study highlighting sigmoid diverticulum perforation secondary to biliary stent migration. We'll explore the background, potential causes, and preventive strategies associated with this complication, aiming to equip you with the knowledge necessary to navigate biliary stent procedures safely.
What Happens When a Stent Strays? Understanding the Risks of Biliary Stent Migration
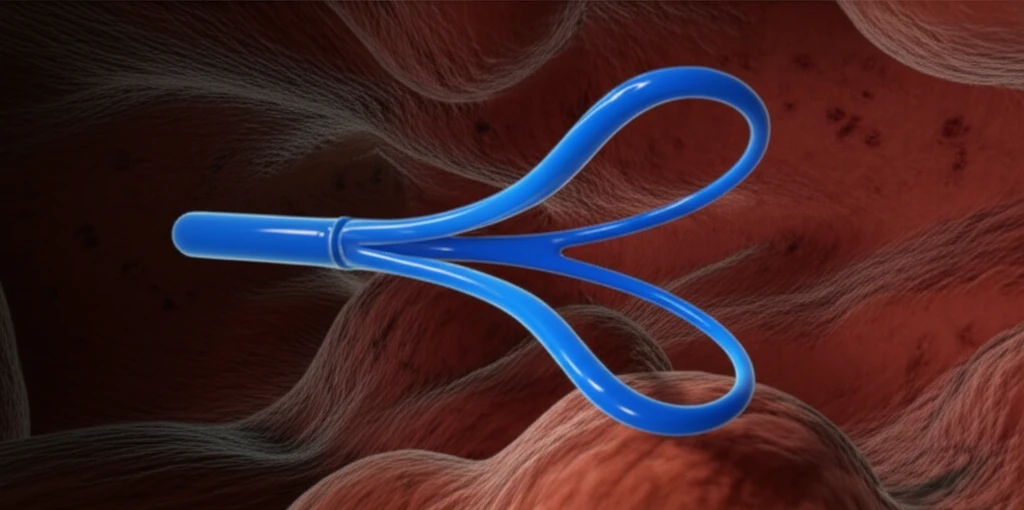
Biliary stent placement, while generally safe, carries a complication rate of 5-10%. The most common issues include cholangitis (bile duct inflammation) and stent obstruction. However, rarer and more severe complications can occur, such as pancreatitis, gastrointestinal bleeding, intestinal perforation, and, notably, biliary stent migration.
- Proximal Migration: Stent moves towards the liver, potentially causing obstruction or damage to the bile ducts.
- Distal Migration: Stent moves through the intestines and is usually excreted. Complications arise if the stent becomes lodged or perforates the intestinal wall.
Preventing Biliary Stent Migration: A Proactive Approach to Patient Safety
Biliary stent migration, although rare, can lead to significant complications. By understanding the risk factors, implementing preventative strategies, and maintaining vigilant post-procedure monitoring, healthcare providers can minimize the likelihood of such events. Patients, too, play a crucial role in recognizing atypical symptoms and seeking prompt medical attention. Together, we can ensure safer and more effective biliary stent procedures, improving patient outcomes and quality of life.
