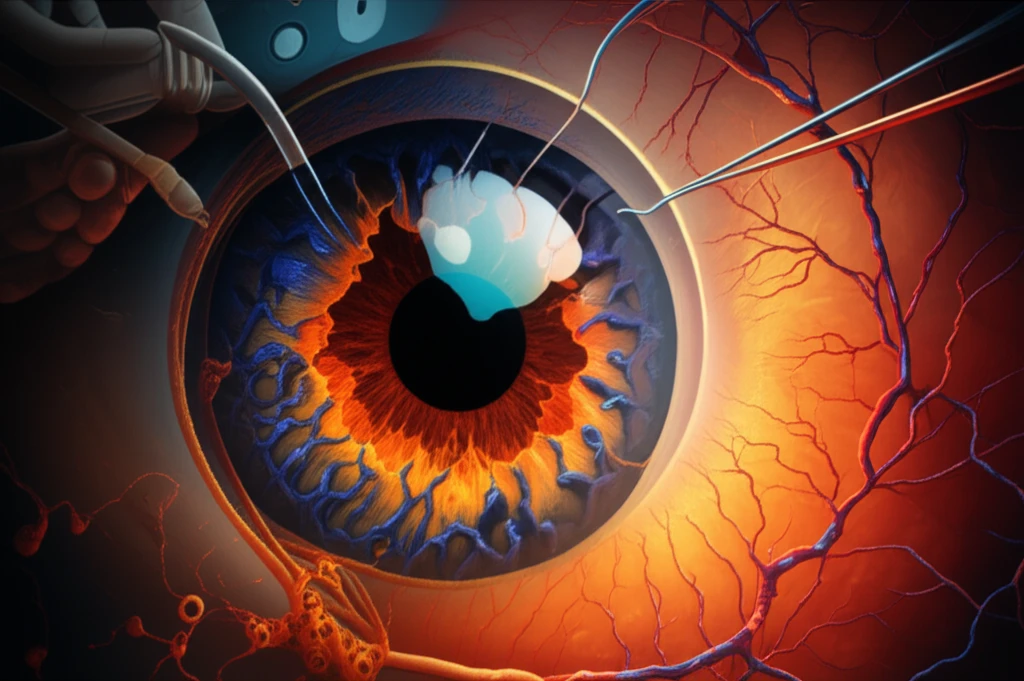
Vision After Cataract Surgery: What You Need to Know About AMD and PCV
"Exploring the impact of cataract surgery on patients with neovascular age-related macular degeneration and polypoidal choroidal vasculopathy."
A recent study highlighted that cataract surgery can lead to improved vision for individuals with neovascular age-related macular degeneration (AMD). Following cataract surgery, patients experienced an improvement in visual acuity, as measured by ETDRS letters. This is encouraging news, as it suggests a potential benefit for those with both cataracts and neovascular AMD.
However, the study also revealed a nuanced picture. While cataract surgery didn't alter the overall frequency of anti-VEGF (vascular endothelial growth factor) injections, a closer look showed that some patients who had been injection-free for over a year prior to cataract surgery needed to resume these injections afterward. Specifically, among 19 patients, 11 required a resumption of anti-VEGF treatment.
This observation raises an important question: are there specific clinical factors or features detectable on optical coherence tomography (OCT) that could help predict which patients might require renewed anti-VEGF injections after cataract surgery? Identifying these factors would be invaluable in optimizing treatment strategies and managing patient expectations.
PCV and the Risk of Submacular Hemorrhage
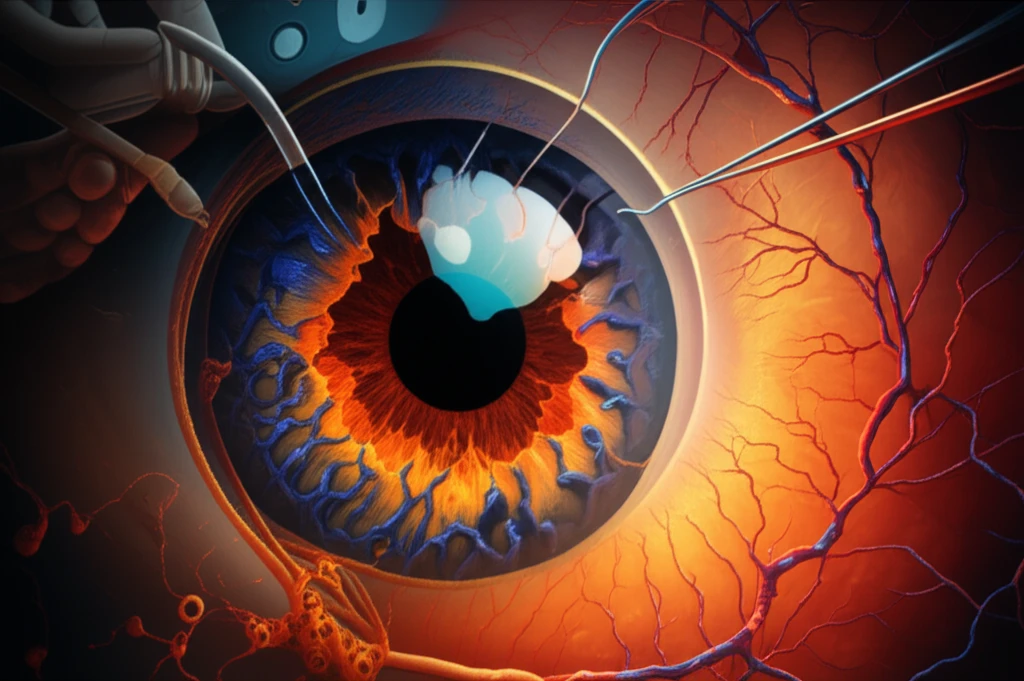
It's important to consider the presence of polypoidal choroidal vasculopathy (PCV), a subtype of AMD that occurs more frequently in Asian populations. One potential complication of active PCV is the development of sudden, massive submacular hemorrhage, which can lead to permanent vision loss.
- Intraocular pressure is known to fluctuate during cataract surgery.
- Shearing forces resulting from these pressure changes may damage choroidal vessels.
- Patients with hypertension and arteriosclerosis may be particularly vulnerable due to increased vessel fragility.
Optimizing Care for AMD and PCV Patients
Cataract surgery can be beneficial for patients with AMD, but careful consideration is necessary, especially in those with PCV. Assessing the activity level of PCV lesions is crucial in determining the optimal management strategy before proceeding with cataract surgery.
Further research is needed to identify clinical factors and OCT features that can predict the need for resumed anti-VEGF injections after cataract surgery. Understanding these factors will enable ophthalmologists to better tailor treatment plans and monitor patients at higher risk.
By carefully evaluating each patient's individual circumstances, including the presence and activity of PCV, ophthalmologists can optimize visual outcomes and minimize the risk of complications following cataract surgery.
