Vasopressors: Are They Harming Your Lungs? What to Know
"A new study reveals surprising differences in how common blood pressure drugs affect pulmonary versus systemic arteries – and why it matters for those with lung issues."
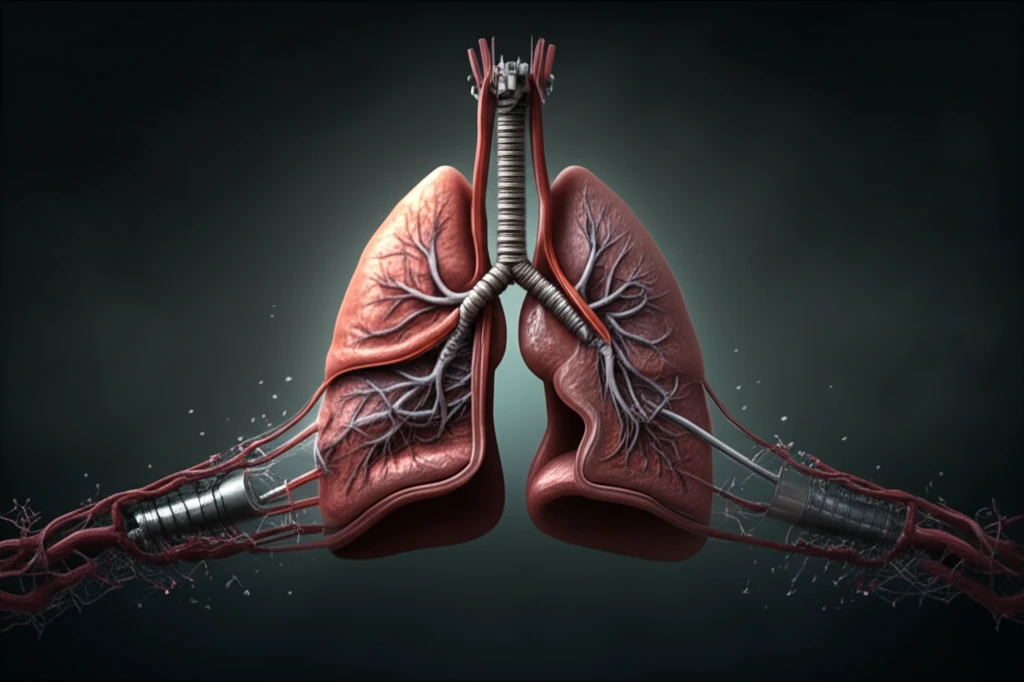
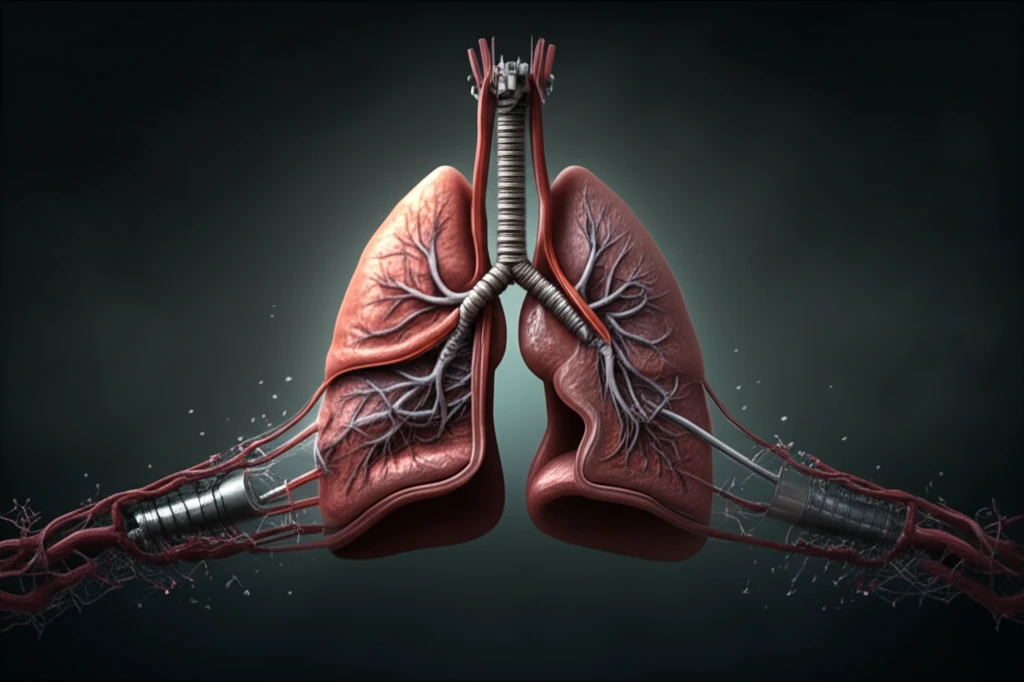
When your blood pressure drops too low, doctors often turn to medications called vasopressors. These drugs help tighten blood vessels, increasing blood pressure and ensuring your organs get enough blood and oxygen. They are crucial in emergency situations and for people with chronic low blood pressure.
However, vasopressors aren't without potential downsides. While they boost blood pressure throughout the body, they can also affect specific areas, like the lungs. This is particularly concerning for individuals with pulmonary hypertension or other lung conditions, where increased pressure in the lungs can worsen their symptoms.
A recent study published in the journal Anesthesiology sheds new light on how different vasopressors affect blood vessels in the lungs versus those in the rest of the body. The findings could influence how doctors choose vasopressors for patients with pre-existing lung problems.
How Do Vasopressors Work?
Vasopressors work by targeting specific receptors on the smooth muscle cells of blood vessels, causing them to constrict. This constriction narrows the vessels, increasing resistance to blood flow and, as a result, raising blood pressure. Different vasopressors target different receptors, leading to variations in their effects.
- Norepinephrine: Primarily acts on alpha-1 adrenergic receptors, causing vasoconstriction.
- Phenylephrine: Another alpha-1 adrenergic agonist, similar to norepinephrine.
- Metaraminol: Also stimulates alpha-1 adrenergic receptors.
- Vasopressin: Acts on V1 receptors, causing vasoconstriction, and is distinct from the others listed above.
Making Informed Decisions About Your Health
The choice of vasopressor is a nuanced decision, and this study provides valuable information for doctors treating patients with pulmonary hypertension or at risk of pulmonary complications. It reinforces the need for personalized treatment strategies that consider the potential impact on both systemic and pulmonary circulation.
