Urethral Stricture Repair: A Simpler Grafting Technique for Better Outcomes
"Discover how preputial mucosal grafts offer an easier and effective alternative to buccal mucosa grafts for urethral stricture repair, especially in resource-limited settings."
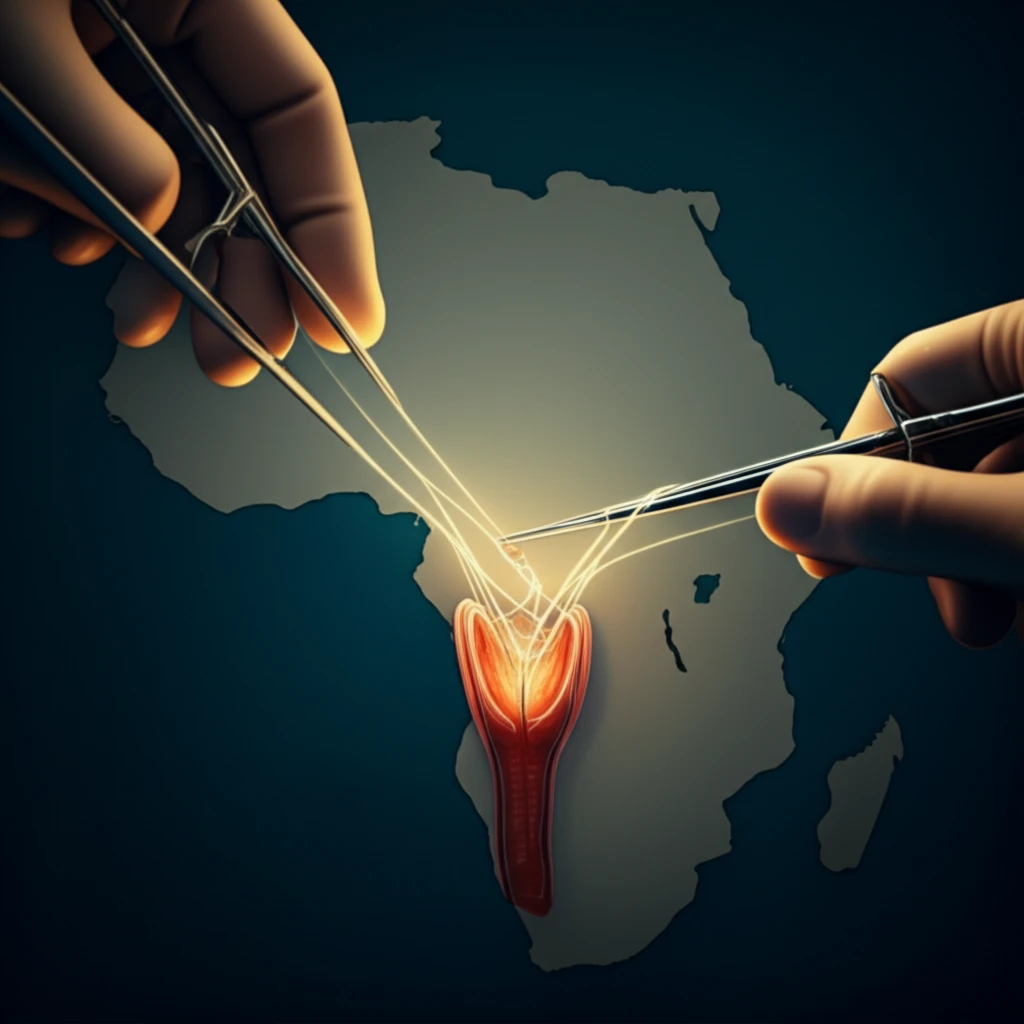
Urethral stricture disease represents a significant health challenge, particularly in sub-Saharan Africa, where it stands as a leading cause of urological morbidity. While developed nations often cite prostate disease as the primary urological concern, the African continent faces a different reality. This divergence is largely attributed to a complex interplay of factors, including the high prevalence of sexually transmitted infections (STIs), rising instances of urethral trauma, and the strain on already over-stretched urological services.
The presence of long-term indwelling urethral catheters, frequently used in the management of prostate disease for extended periods (sometimes up to two years), further compounds the problem. This prolonged catheterization significantly elevates the risk of developing urethral strictures, creating a vicious cycle of urological complications. The predominant cause of these strictures is often attributed to sexually transmitted infections, particularly those involving gonococcus or chlamydia.
These infections frequently lead to the development of long and severe strictures characterized by spongiofibrosis, a condition where scar tissue replaces healthy tissue. This is especially common in the anterior urethra, the region where the periurethral glands are located. Unfortunately, these types of strictures often prove resistant to conventional treatments such as urethral dilatation, optical urethrotomy, or primary anastomosis. As a result, the majority of strictures in Africa are most effectively managed through open substitution urethroplasty, a surgical procedure that involves replacing the damaged section of the urethra with healthy tissue.
Why Preputial Mucosal Grafts Offer a Viable Solution
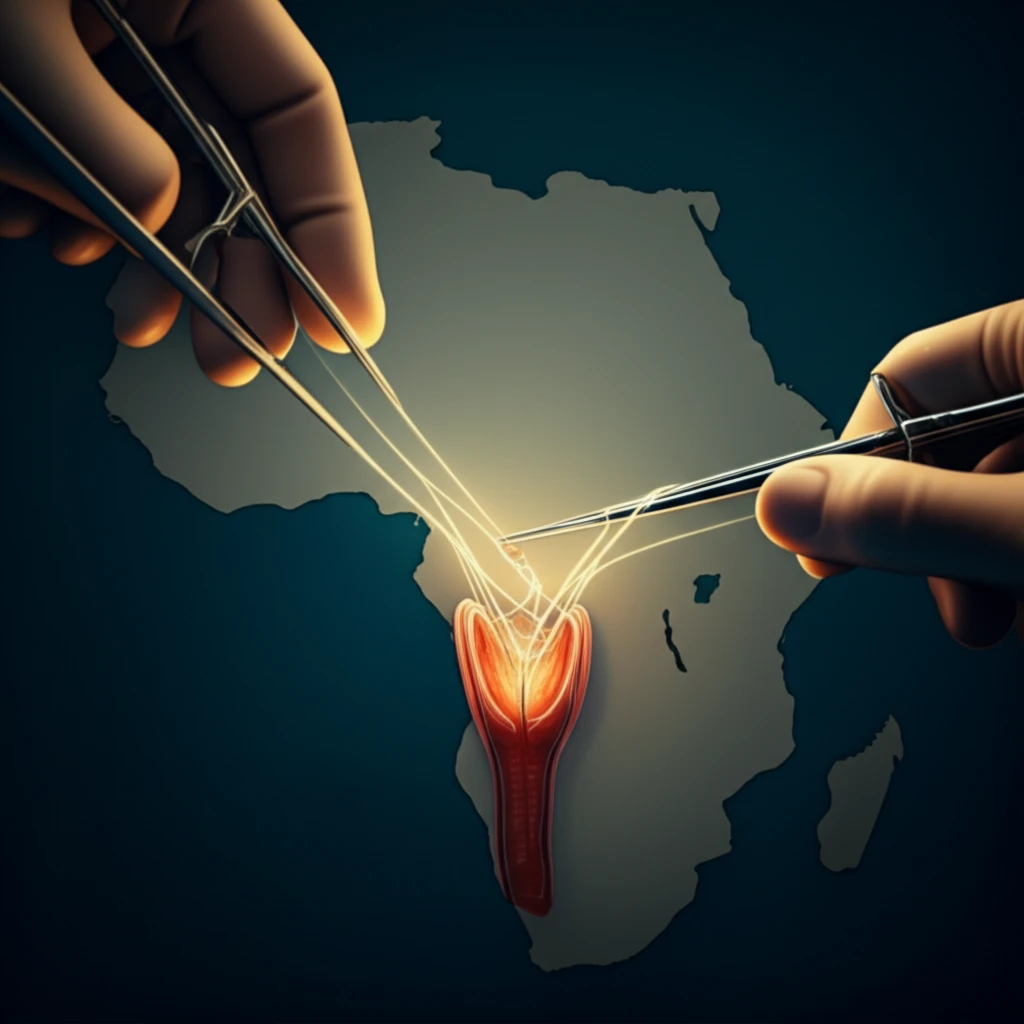
The gold standard for substitution urethroplasty has traditionally been the use of buccal mucosa grafts (BMG), which involves harvesting tissue from the lining of the mouth. While effective, this procedure presents considerable challenges in resource-limited settings. These challenges include the need for specialized equipment, longer operating times, and the requirement for general anesthesia and intubation.
- Simplified Procedure: The preputial graft technique is technically less demanding compared to buccal mucosa grafts.
- Reduced Operating Time: Harvesting preputial tissue generally requires less time than harvesting buccal mucosa.
- Lower Anesthesia Requirements: The procedure can often be performed under local or regional anesthesia, reducing the risks associated with general anesthesia.
- Good Clinical Outcomes: Studies have demonstrated that preputial grafts can achieve comparable success rates to buccal mucosa grafts in treating urethral strictures.
A Promising Avenue for Improved Urological Care
The high incidence and severity of urethral strictures in Africa necessitate the adoption of innovative approaches to mitigate morbidity. The utilization of PMG represents a valuable strategy for reducing the burden of urethral stricture disease, particularly in resource-constrained environments. As healthcare systems strive to enhance accessibility and optimize patient outcomes, simplified yet effective techniques like preputial grafting hold significant promise for improving urological care in Africa and beyond.
