Unstable Plaques: How Oxidized Lipids Trigger Artery Trouble
"Discover how common substances found in artery plaques, 27-hydroxycholesterol and 4-hydroxynonenal, worsen the condition and what you can do."
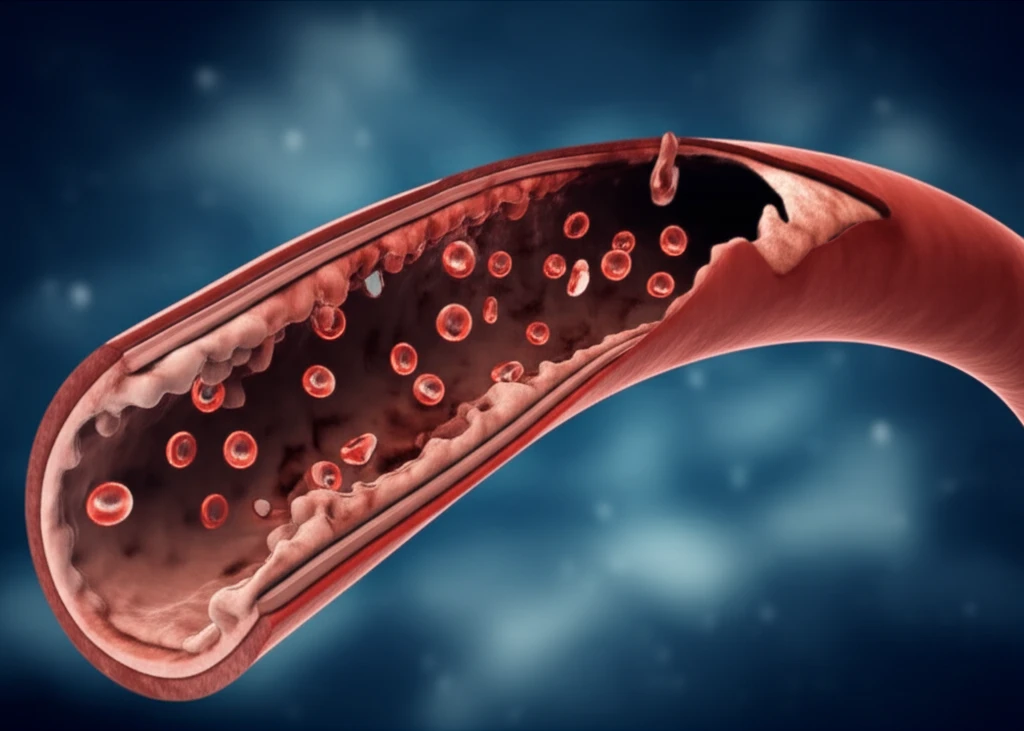
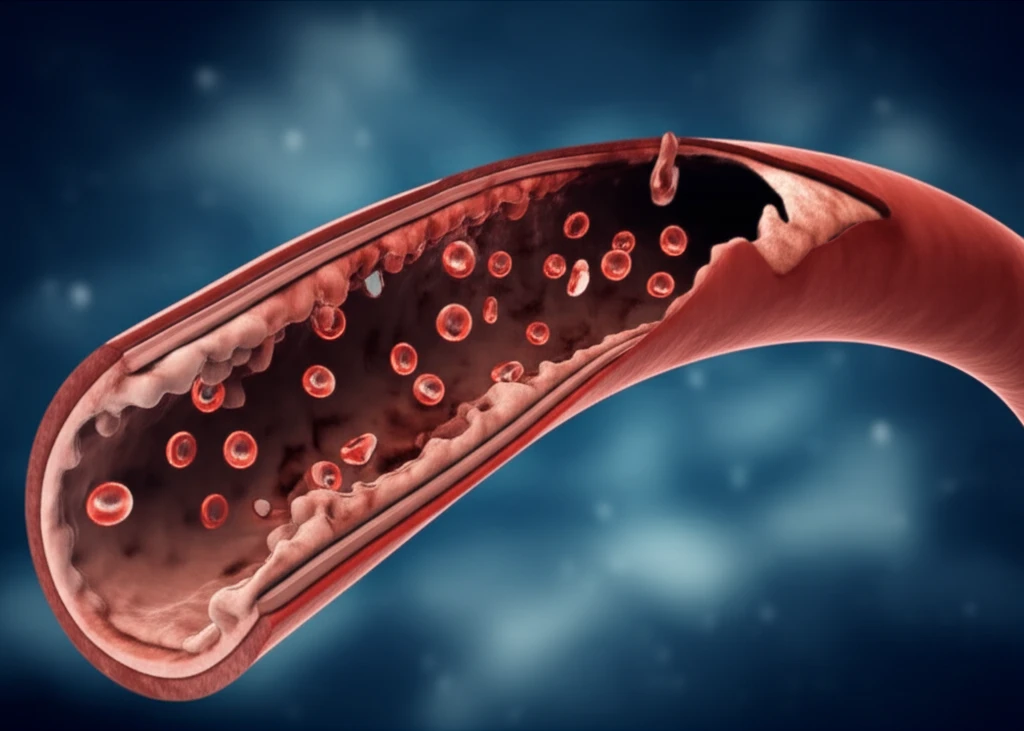
Atherosclerosis is more than just clogged arteries; it's a complex inflammatory process that can lead to serious heart problems. One of the key factors involved in the progression of this disease is the activity of an enzyme system known as cyclooxygenase 2/membrane-bound prostaglandin E synthase 1 (COX-2/mPGES-1). When this system is overactive, it contributes to the instability of plaques, increasing the risk of rupture.
A major cause of this overactivity is the presence of oxidized lipids – harmful fats that accumulate when low-density lipoproteins (LDLs, or "bad" cholesterol) become damaged. Two specific oxidized lipids, 27-hydroxycholesterol (27-OH) and 4-hydroxynonenal (HNE), are found in high concentrations within atherosclerotic plaques. Researchers are working to understand exactly how these lipids contribute to plaque progression and instability.
New research sheds light on how 27-OH and HNE promote the up-regulation of COX-2 and mPGES-1. This, in turn, leads to increased production of a hormone-like substance called prostaglandin E2 (PGE2), as well as increased nitric oxide. This study will explore how those factors contribute to inflammation and matrix metalloproteinase production by activated macrophages which may cause eventual rupture of plaque contributing to matrix metalloproteinase production.
How 27-OH and HNE Fuel Artery Inflammation
The study focused on how 27-OH and HNE impact key inflammatory processes within cells. Researchers discovered that both 27-OH and HNE cause an increase in the production of COX-2 and mPGES-1 enzymes. This is a critical step because these enzymes work together to produce prostaglandin E2 (PGE2), a molecule known to promote inflammation.
- COX-2 and mPGES-1 Up-Regulation: Both 27-OH and HNE significantly increased COX-2 protein levels in the cells. Similarly, mPGES-1 mRNA levels and protein levels also rose with exposure to these oxidized lipids, particularly HNE.
- PGE2 Production: The increased activity of COX-2 and mPGES-1 led to a corresponding surge in PGE2 production. PGE2 is a potent inflammatory mediator implicated in various stages of atherosclerosis.
- iNOS and Nitric Oxide: Expression of inducible nitric oxide synthase (iNOS) increased as a result of 27-OH and HNE treatments; nitric oxide (NO) production also increased.
Taking Control of Your Artery Health
The research highlights the importance of managing oxidized lipids to protect your arteries. While 27-OH and HNE are produced within the body during LDL oxidation, lifestyle and dietary choices can significantly influence this process.
Here are key strategies to consider: <ul><li><b>Antioxidant-Rich Diet:</b> Consume plenty of fruits, vegetables, and other foods rich in antioxidants. Antioxidants can help protect LDL cholesterol from oxidation, reducing the formation of harmful oxidized lipids.</li><li><b>Limit Processed Foods:</b> Processed foods often contain high levels of unhealthy fats that are prone to oxidation. Reduce your intake of fried foods, processed meats, and sugary snacks.</li><li><b>Manage Cholesterol:</b> Work with your doctor to manage your overall cholesterol levels. This may involve dietary changes, exercise, or medication if necessary.</li><li><b>Anti-inflammatory agents:</b> Natural anti-inflammatory options such as EGCG is capable of improving plaque stability.</li></ul>
By addressing the factors that contribute to oxidized lipid formation and supporting healthy inflammatory responses, you can take proactive steps to promote artery health and reduce your risk of atherosclerosis.
