Unmasking the Anti-Vax Movement: What the Data Reveals About Vaccine Exemptions and Public Health
"A Deep Dive into Nonmedical Exemptions, Hotspots, and the Ongoing Battle Against Vaccine Hesitancy."
In a world grappling with health crises and scientific advancements, the debate around vaccines remains a persistent challenge. This article revisits a comprehensive study, "The state of the antivaccine movement in the United States: A focused examination of nonmedical exemptions in states and counties," originally published in PLOS Medicine. This analysis provides critical insights into the ongoing battle against vaccine hesitancy and its potential impact on public health, especially within specific communities.
Vaccine hesitancy isn't just a matter of personal choice; it's a complex issue with far-reaching consequences for public health. As the medical community continues to emphasize the safety and efficacy of vaccines, understanding the factors that contribute to vaccine refusal becomes increasingly important. This article examines the data, trends, and potential implications of nonmedical exemptions (NMEs) across the United States, focusing on key areas where vaccine hesitancy poses a significant risk.
The information presented here serves as a starting point for a deeper understanding of vaccine hesitancy. By exploring the data, trends, and potential implications, readers can gain a more informed perspective on this complex issue. Let's explore the key findings, analyze the implications, and consider the path forward in this critical area of public health.
Unpacking the Data: Key Findings on Nonmedical Exemptions
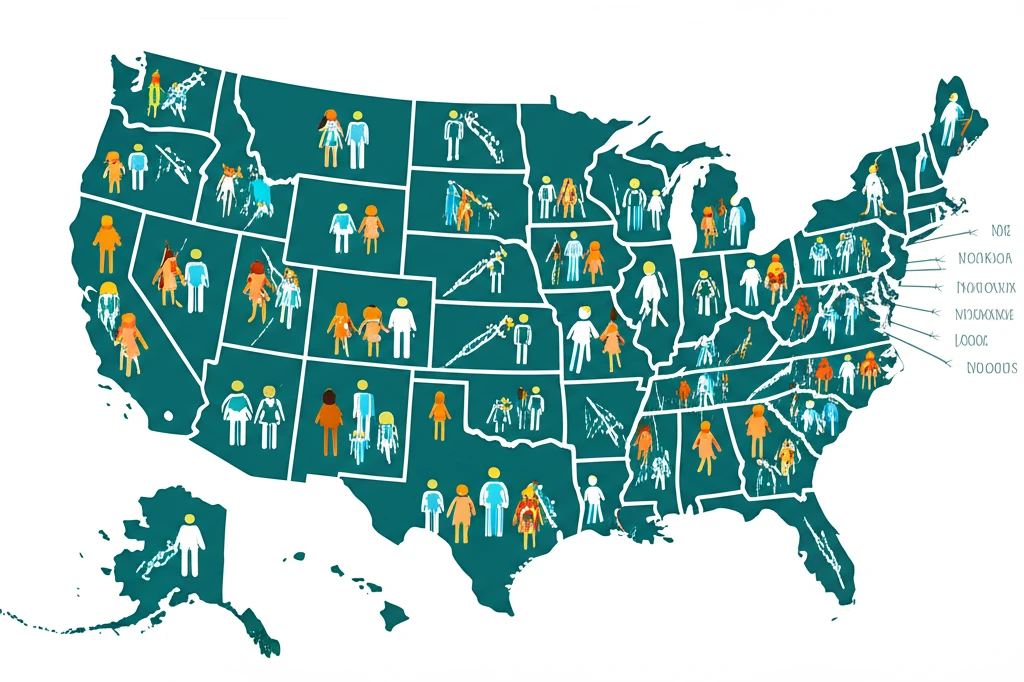
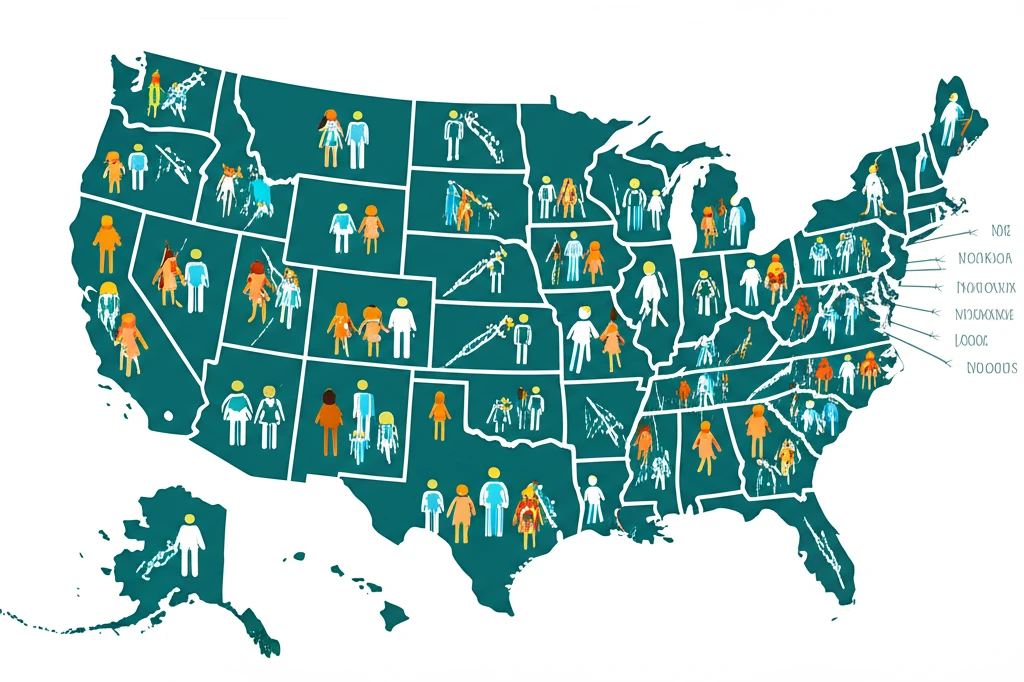
The original study identified significant trends in nonmedical exemptions (NMEs) across the United States. The data revealed a rise in philosophical-belief exemptions in several states, specifically those allowing this policy. This rise suggests an increase in vaccine hesitancy among certain populations. Understanding these trends is crucial for public health professionals to identify areas of concern and implement targeted interventions.
- Maricopa County, Arizona: 2,947 NMEs.
- Salt Lake County, Utah: 956 NMEs.
- King County, Washington: 940 NMEs.
- Multnomah County, Oregon: 711 NMEs.
- Oakland County, Michigan: 686 NMEs.
Moving Forward: Addressing Vaccine Hesitancy and Protecting Public Health
This analysis serves as a reminder that protecting public health requires ongoing vigilance, data-driven strategies, and a commitment to evidence-based practices. It's a complex issue, but by working together, we can strive toward a healthier and safer future for all. This includes accurate information and resources for families to promote informed decision-making and community well-being.
