Unlocking the Secrets: How Lipoproteins and Toll-Like Receptor 2 Impact Staphylococcus aureus Infections
"Delve into the crucial role of lipoproteins and Toll-Like Receptor 2 in the pathogenesis of Staphylococcus aureus, and what this means for future treatments."
Staphylococcus aureus, a common bacterium, is responsible for a wide range of infections, from minor skin irritations to life-threatening conditions like sepsis and pneumonia. Understanding how this bacterium invades and establishes infections within the human body is crucial for developing effective treatments and preventive strategies.
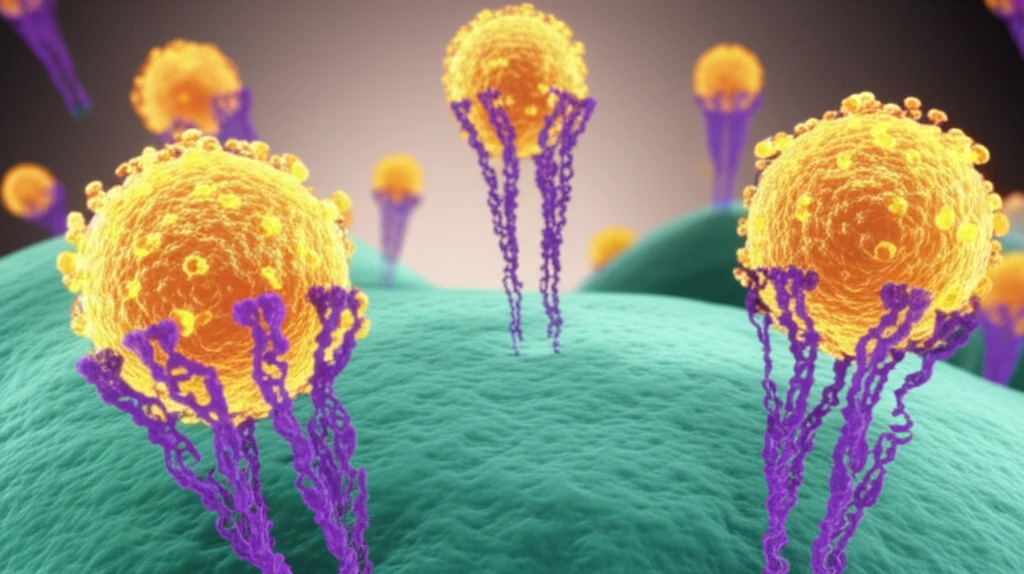
Recent research has focused on the intricate interactions between Staphylococcus aureus and the host's immune system, particularly the role of Toll-Like Receptor 2 (TLR2) and lipoproteins. These components are key players in the body's defense mechanisms, but S. aureus has evolved strategies to exploit them for its own benefit.
This article delves into the groundbreaking findings of Nguyen et al., which illuminate how lipoproteins and TLR2 facilitate the invasion of Staphylococcus aureus into epithelial cells. By understanding these mechanisms, we can pave the way for innovative therapeutic interventions that target these specific interactions, ultimately reducing the burden of S. aureus infections.
How Lipoproteins and TLR2 Enhance Staphylococcus aureus Invasion
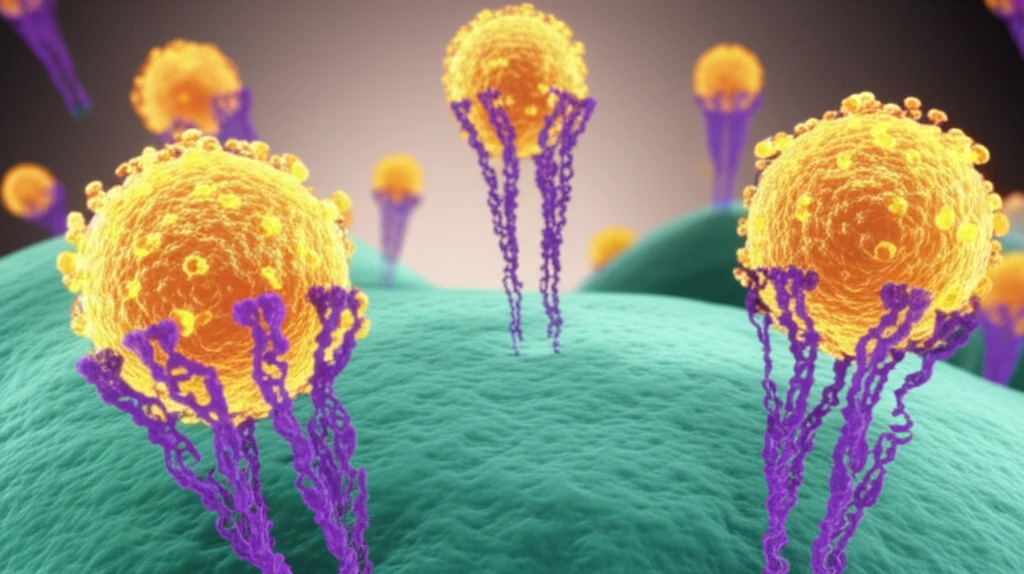
The study by Nguyen et al. highlights the critical role of lipoproteins, which are molecules composed of lipids and proteins, in enhancing the ability of Staphylococcus aureus to invade epithelial cells. Epithelial cells form the lining of various tissues and organs, serving as the first line of defense against pathogens. When S. aureus encounters these cells, it needs to breach this barrier to establish an infection.
- Lipoprotein Binding: Lipoproteins on the surface of S. aureus bind to TLR2 on epithelial cells.
- Enhanced Adhesion: This binding enhances the adhesion of the bacteria to the epithelial cells, making it easier for them to attach and initiate the invasion process.
- Cellular Entry: The interaction facilitates the entry of S. aureus into the epithelial cells, allowing the bacteria to hide from the immune system and establish a persistent infection.
Implications for Future Treatments
The findings from Nguyen et al. provide valuable insights into the mechanisms by which Staphylococcus aureus invades epithelial cells, opening new avenues for therapeutic intervention. Targeting the interaction between lipoproteins and TLR2 could disrupt the invasion process and prevent the establishment of infections. Potential strategies include developing drugs that block the binding of lipoproteins to TLR2, or that modulate the TLR2 signaling pathway to enhance the host's immune response without causing excessive inflammation. Further research is needed to translate these findings into effective clinical treatments, but the potential impact on reducing the burden of S. aureus infections is significant.
