Unlocking Psoriatic Arthritis Treatment: Navigating Biologic Therapies for Long-Term Relief
"A comprehensive look at anti-TNFα biologics for psoriatic arthritis: treatment patterns, costs, and real-world insights."
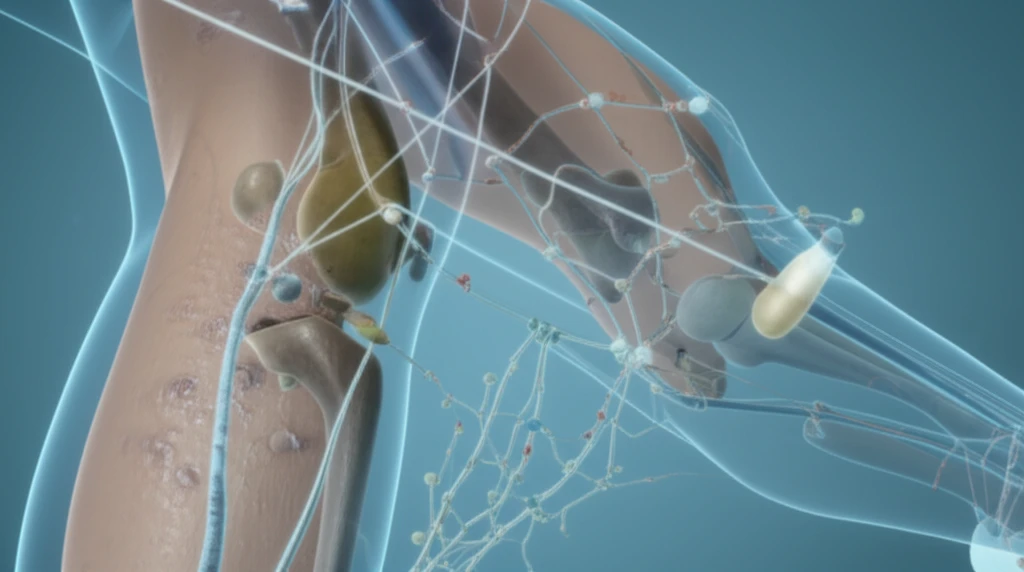
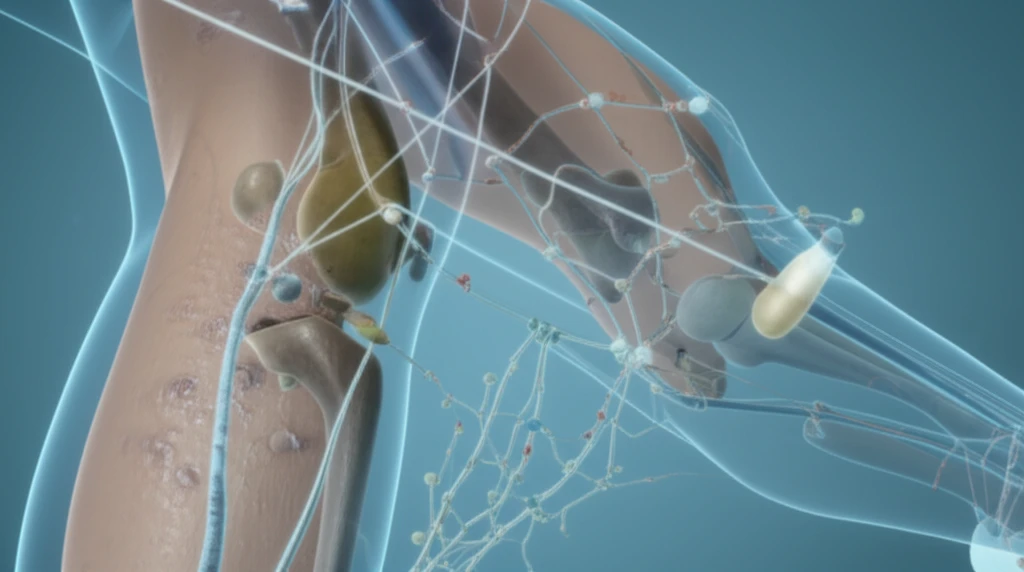
Psoriatic Arthritis (PsA) presents a unique challenge in the realm of autoimmune disorders. It intricately intertwines joint inflammation, skin lesions, and a myriad of other symptoms that can significantly impact the quality of life. Managing PsA effectively requires a comprehensive approach, often involving biologic therapies such as anti-tumor necrosis factor alpha (anti-TNFα) drugs. As these treatments evolve, understanding their patterns of use and associated costs becomes increasingly vital.
The journey through PsA treatment often begins with conventional therapies aimed at alleviating immediate symptoms. However, when these approaches fall short, anti-TNFα biologics emerge as a beacon of hope. These advanced medications target specific proteins in the immune system to reduce inflammation and slow disease progression. Yet, with various anti-TNFα options available, navigating the treatment landscape can be complex.
In a recent study, researchers delved into the real-world usage of anti-TNFα biologic therapies among PsA patients in the United States. By examining treatment patterns, costs, and factors influencing treatment choices, the study sheds light on the practical considerations for managing PsA with these powerful medications. The insights gleaned from this study offer valuable guidance for healthcare providers and individuals seeking to optimize their PsA treatment strategies.
Anti-TNFα Biologics: How Treatment Patterns Evolve Over Time?
The study, which analyzed data from nearly 1,000 PsA patients initiating anti-TNFα therapy, revealed a fascinating trend: while most patients remained on a single line of therapy, a notable subset transitioned through multiple lines of treatment during the three-year follow-up period. This observation underscores the dynamic nature of PsA management and the need for personalized treatment strategies.
- First-Line Therapy: Patients averaged approximately 17 months before switching.
- Second/Third-Line Therapies: Persistence on each line decreased, suggesting evolving treatment needs.
What Does This Mean For PsA?
Overall, this study provides valuable insights into the real-world utilization of anti-TNFα biologic therapies for PsA. By understanding treatment patterns, costs, and factors influencing treatment choices, healthcare providers and patients can work together to optimize outcomes and improve the lives of individuals living with PsA. Further research is needed to explore the reasons behind treatment switching and to identify predictors of long-term treatment success.
