Unlocking Kidney Health: How C5aR1 Research Offers New Hope for Fibrosis Treatment
"Groundbreaking study reveals the potential of targeting C5aR1 in Foxd1+ stromal cells to combat kidney fibrosis, offering a beacon of hope for future therapies."
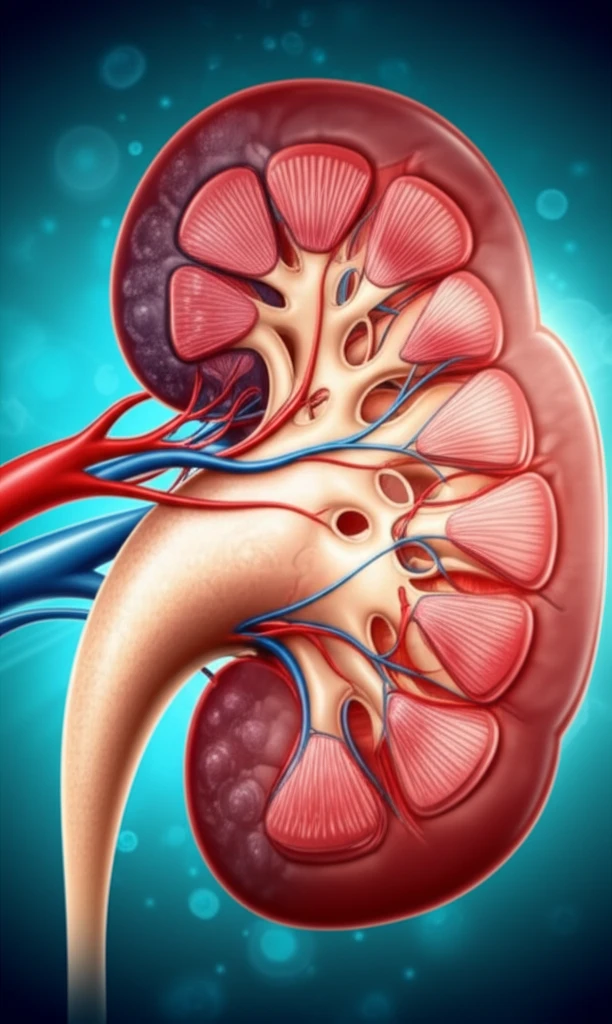
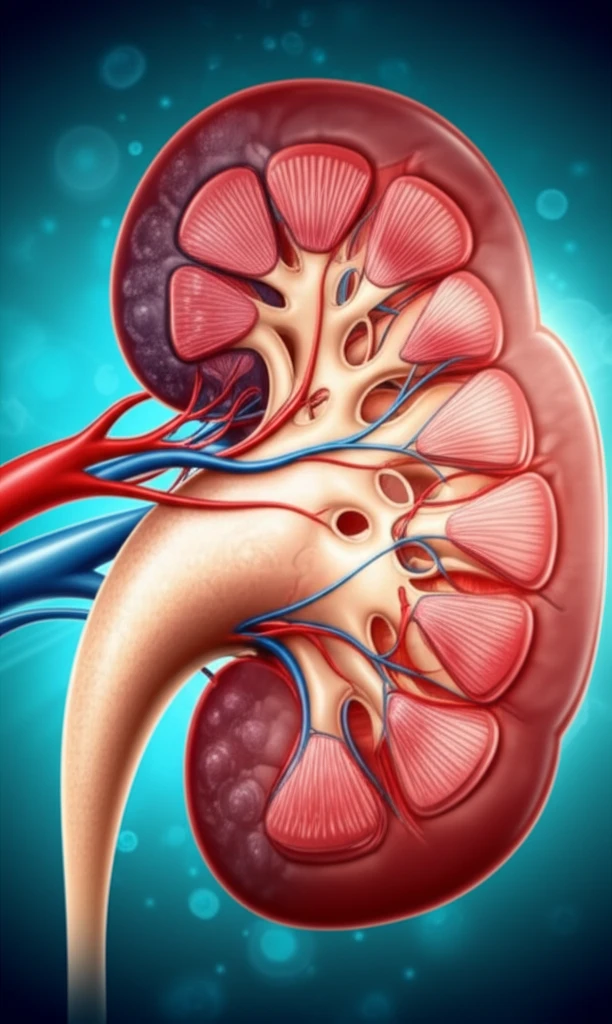
Kidney fibrosis, the scarring of kidney tissue, is a common endpoint of many chronic kidney diseases. It impairs kidney function and can ultimately lead to kidney failure. Understanding the mechanisms that drive fibrosis is crucial for developing effective treatments.
Recent research has focused on the role of perivascular mesenchymal cells, also known as resident fibroblasts or pericytes, in kidney fibrosis. These cells, which express the transcription factor Foxd1, are now recognized as key players in the development of interstitial myofibroblasts, the cells responsible for excessive matrix deposition in fibrotic kidneys.
A groundbreaking study sheds light on the role of the anaphylatoxin receptor C5aR1 in these Foxd1-expressing cells. Published in Molecular Immunology, the research demonstrates that reducing C5aR1 in these specific cells can significantly reduce kidney fibrosis. This discovery opens new avenues for targeted therapies aimed at preserving kidney function and improving patient outcomes.
C5aR1: A Key Target in the Fight Against Kidney Fibrosis
The study highlights the potential of C5aR1 as a therapeutic target. C5aR1 is a receptor for the complement protein C5a, a potent inflammatory mediator. Previous research has shown that C5aR1 contributes to inflammation and fibrosis in various tissues, including the kidney.
- Reduced Inflammation: The study showed that mice lacking C5aR1 in Foxd1-expressing cells had reduced inflammation in their kidneys after injury.
- Decreased Fibrosis: These mice also exhibited less kidney fibrosis compared to control mice.
- Reduced Cytokine Production: In vitro experiments showed that pericytes lacking C5aR1 produced fewer inflammatory cytokines, suggesting a direct role for C5aR1 in promoting inflammation in these cells.
The Future of Kidney Disease Treatment
This research provides a compelling rationale for developing therapies that target C5aR1 in Foxd1-expressing cells. While further studies are needed to translate these findings into clinical applications, the results offer a promising new direction for the treatment of kidney fibrosis. By specifically targeting the cells that contribute to fibrosis, future therapies may be able to prevent or reverse kidney damage, ultimately improving the lives of individuals with chronic kidney disease.
