Unlocking Heart Health: How a Common Immune Response Could Change Everything
"New research reveals surprising connections between the immune system and blood vessel function, offering fresh insights into preventing heart disease."
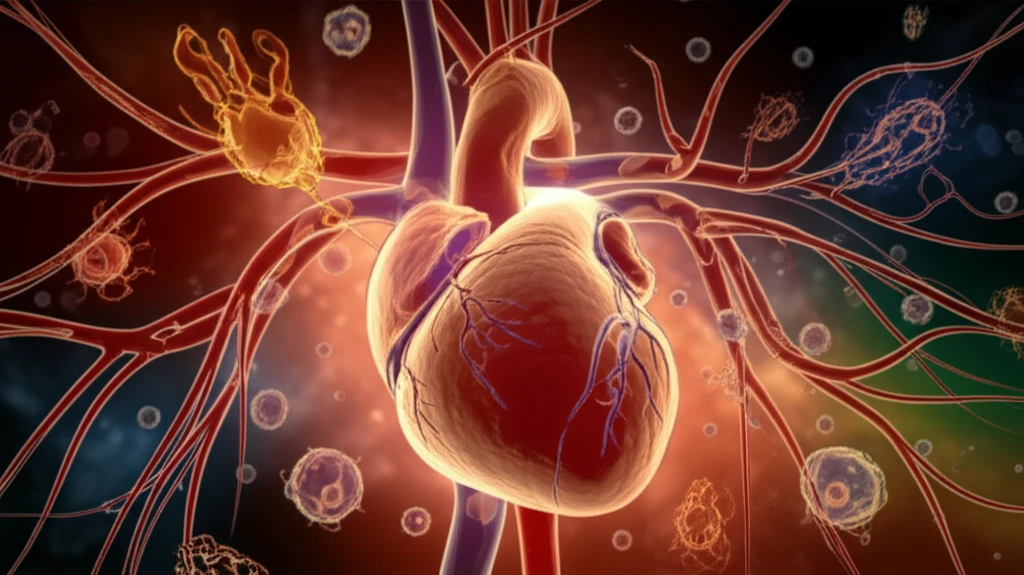
The heart, a tireless engine of life, is often at the forefront of our health concerns. Cardiovascular diseases, encompassing a range of conditions like heart attacks and strokes, remain a leading cause of mortality globally. While factors like diet, exercise, and genetics are well-known contributors, a new frontier in heart health is emerging: the intricate relationship between our immune system and the health of our blood vessels.
Recent studies have illuminated the crucial role the immune system plays in vascular function. One area of particular interest involves the body's response to perceived threats, like viral infections. This response, mediated by the immune system, can trigger inflammatory processes. However, excessive or chronic inflammation can wreak havoc on our blood vessels, contributing to conditions like atherosclerosis, where arteries become clogged with plaque.
This article explores a fascinating study that uncovers a surprising connection between the immune response and the ability of blood vessels to relax. We will explore how a specific immune pathway, often activated during infections, impacts the crucial process of blood vessel relaxation, which is essential for maintaining healthy blood flow. By understanding this connection, we can gain valuable insights into how to protect our cardiovascular health.
The Immune System's Role in Vascular Health: A Deep Dive
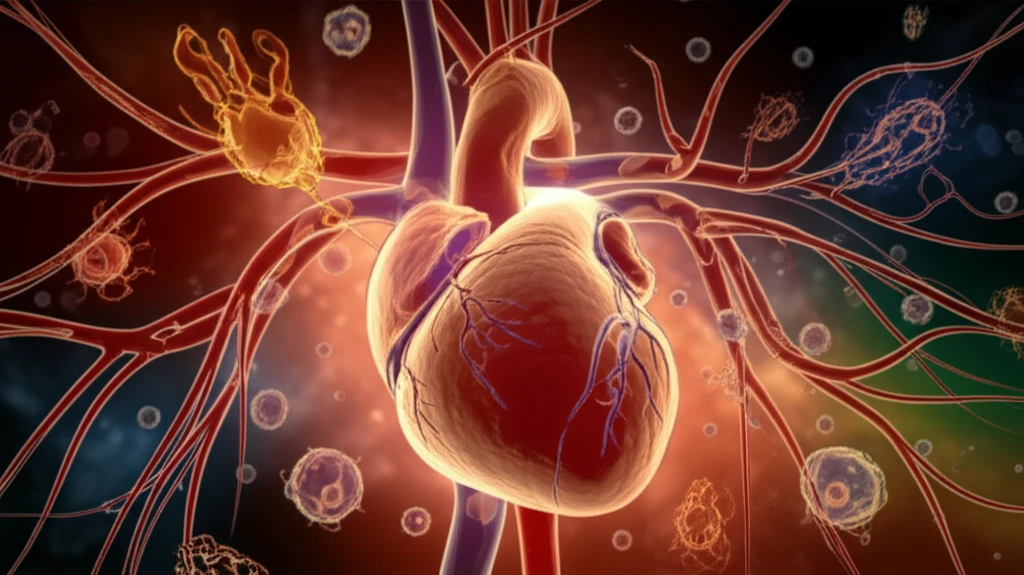
To grasp the impact of immune responses on blood vessels, consider the example of a common immune pathway triggered by substances like viral double-stranded RNA (dsRNA). The body recognizes these dsRNAs through receptors like TLR3. This recognition sets off a chain reaction, prompting the release of inflammatory signals and the activation of immune cells. This process, while protective in the face of infection, can sometimes go awry, leading to vascular dysfunction.
- Vascular Dysfunction: dsRNA exposure leads to a decrease in the blood vessels' ability to widen, which contributes to the formation of cardiovascular diseases.
- Inflammation and Blood Vessels: Excessive or chronic inflammation can wreak havoc on our blood vessels, contributing to conditions like atherosclerosis, where arteries become clogged with plaque.
- Immune Response: The body recognizes these dsRNAs through receptors like TLR3. This recognition sets off a chain reaction, prompting the release of inflammatory signals and the activation of immune cells.
Implications and Future Directions
The study's findings open doors to potential therapeutic strategies. By understanding how the immune response impacts blood vessel function, researchers can explore ways to modulate these pathways and protect against cardiovascular disease. This includes investigating targeted therapies that can either dampen excessive inflammation or restore normal NO signaling. The knowledge gained from this research not only improves our understanding of heart health but also paves the way for innovative preventive and therapeutic measures in the future. The interplay between our immune system and vascular health is a critical area for protecting our cardiovascular health.
