Tirofiban: Can This Drug Improve Outcomes in Emergency Heart Procedures?
"Discover how tirofiban, a platelet aggregation inhibitor, is being explored to enhance myocardial perfusion and cardiac function during emergency angioplasty."
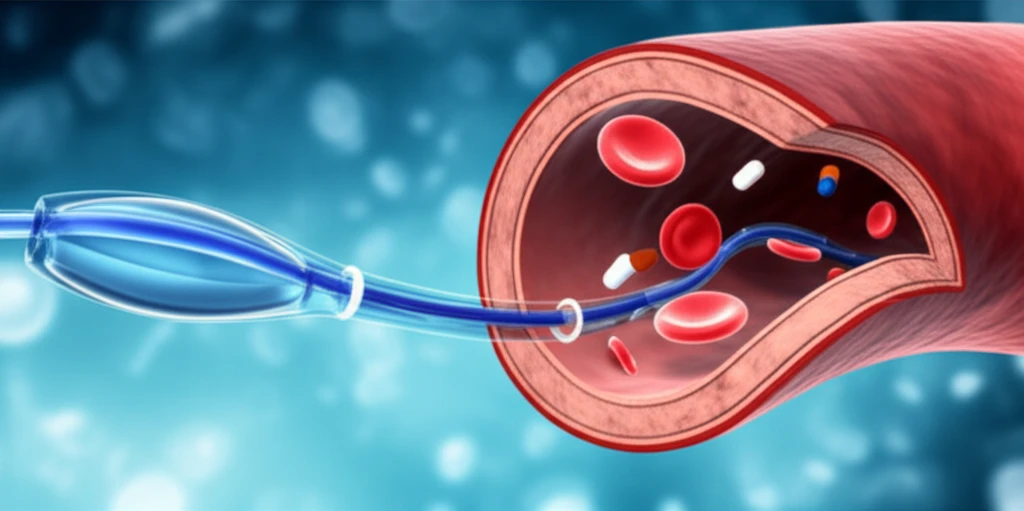
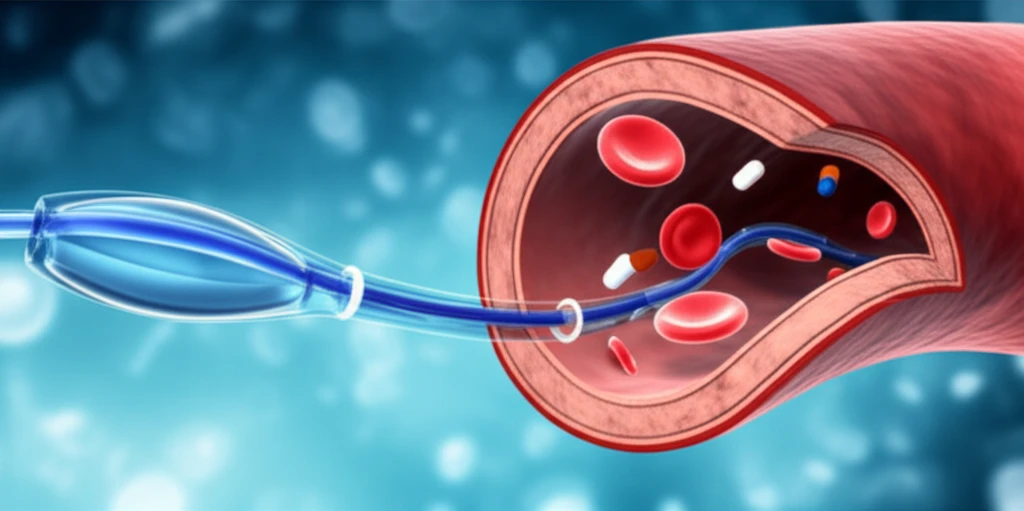
When a coronary artery becomes blocked, often due to plaque rupture and subsequent clot formation, it leads to a heart attack. Platelets, tiny blood cells that clump together to form clots, play a critical role in this process. That’s where tirofiban comes in. Tirofiban is a medication that blocks platelet aggregation, helping to prevent further clot formation during these critical events.
Emergency percutaneous coronary intervention (PCI), or angioplasty, is a life-saving procedure used to open blocked coronary arteries. During PCI, a cardiologist inserts a catheter with a balloon into the blocked artery, inflates the balloon to widen the artery, and often places a stent to keep it open. However, even with PCI, complications like distal microcirculation embolism (small clots blocking tiny vessels) and no-reflow (failure of blood to flow properly after the blockage is opened) can occur.
A study published in Genetics and Molecular Research investigated the use of tirofiban during emergency PCI to see if it could improve blood flow and protect the heart. The researchers focused on tirofiban's effects on platelet alpha-granule membrane protein (GMP-140), a marker of platelet activation, and its impact on myocardial perfusion (blood flow to the heart muscle).
How Does Tirofiban Help During Emergency PCI?
The study randomly divided 70 patients undergoing emergency PCI into two groups: a tirofiban group and a control group. The tirofiban group received an intracoronary injection of tirofiban after the initial balloon dilation of the blocked artery but before stent placement. The control group underwent standard PCI procedures without tirofiban.
- GMP-140 Levels: Measured before and 12 hours after surgery to assess platelet activation.
- Troponin I (cTnI) Levels: Measured before and 12 hours after surgery to assess heart muscle damage.
- N-terminal pro-brain natriuretic peptide (NT-proBNP) Levels: Measured 1 and 7 days after surgery to assess heart function.
Future of Tirofiban in Cardiac Care
The study's findings suggest that tirofiban can be a valuable addition to emergency PCI, improving blood flow and reducing heart muscle damage. While this study provides important insights, further research is needed to confirm these benefits and determine the optimal way to use tirofiban in emergency cardiac care. Future studies could compare intracoronary tirofiban with intravenous administration and include a larger, more diverse patient population.
