Tiny Capsules, Big Impact: Can Nanotechnology Conquer AIDS Drug Delivery?
"Scientists are exploring how nanotechnology can improve the effectiveness and availability of Lopinavir, a crucial anti-AIDS drug, offering hope for better treatment outcomes."
The global fight against Acquired Immune Deficiency Syndrome (AIDS) continues, with millions affected worldwide, particularly in resource-limited countries. Significant progress has been made in antiretroviral therapy, utilizing several classes of agents, including nucleotide reverse transcriptase inhibitors (NRTIs), non-NRTIs (NNRTIs), protease inhibitors (PIs), and integrase inhibitors. Effective treatment often involves a combination of three to four potent agents tailored to the individual, reducing viral load and improving the patient’s T-lymphocyte count.
However, administering multiple drugs (poly-pharmacy) can lead to complex drug interactions. For example, NNRTIs and PIs are metabolized by the CYP450 enzyme system, predominantly the 3A4 isoform, resulting in pharmacokinetic complications. Many of these drugs act as both substrates and modulators of CYP3A4, making interactions unpredictable. Ritonavir (RTV), a PI with high oral bioavailability, serves as a strong CYP3A inhibitor, often used to boost the effectiveness of other drugs.
Lopinavir (LPV), an analog of RTV, was designed to better interact with mutated HIV protease. While LPV is effective against both wild-type and mutated HIV, it suffers from low oral bioavailability due to P-glycoprotein (P-gp) and multidrug resistance-associated protein 2 (MRP2) efflux, as well as extensive pre-systemic metabolism by CYP3A4. This process primarily occurs in the enterocytes of the intestine, reducing plasma levels and effectiveness. Co-administration of LPV with low-dose RTV improves absorption but introduces drawbacks such as increased toxicity and gastrointestinal disturbances.
The Nano-Micro Solution: How It Works
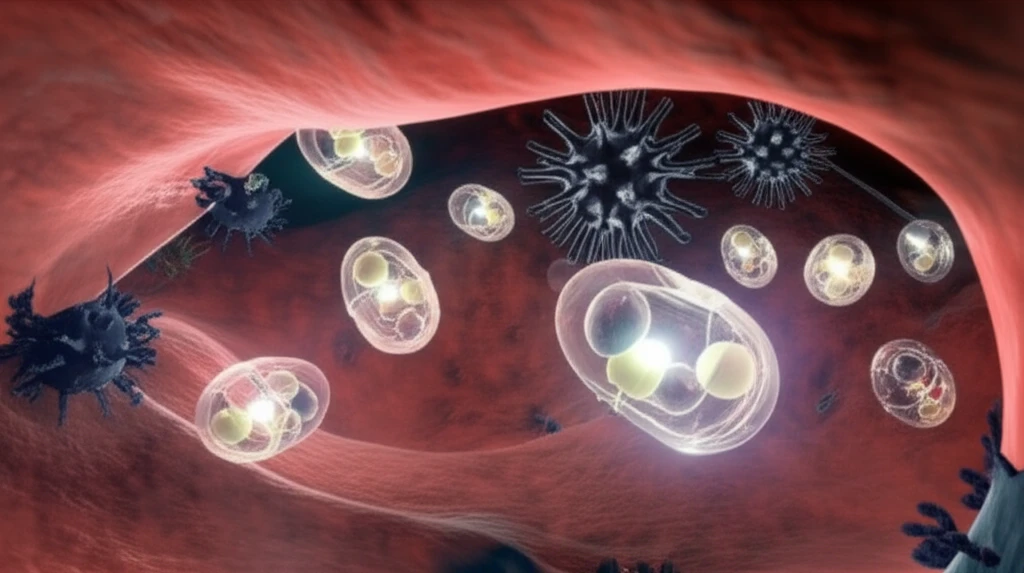
To address these challenges, researchers have explored novel therapeutic delivery systems for LPV that avoid the need for concomitant RTV administration. One promising approach involves encapsulating LPV within biodegradable PLGA nanocapsules (NCs) that are themselves embedded in gastro-resistant bio-adhesive microparticles (MCPs). This “Trojan horse” strategy aims to bypass P-gp efflux and protect the drug from CYP3A pre-systemic metabolism. The study by Nassar et al. (2018) delves into this method, examining how the characteristics of the NC wall, the oil core, and drug load within the MCPs influence LPV absorption without RTV.
- F[I]: Composed of OA NCs embedded in MCPs, with a specific ratio of oleic acid (OA), Labrafil M 1944 CS, PLGA, and LPV.
- F[II]: Similar to F[I] but with a higher PLGA content to create a thicker NC coating.
- F[III]: Prepared with one-third of the ingredient quantities used in F[II], also aimed at examining the significance of NC coating thickness.
Looking Ahead: Potential for Improved HIV Treatment
The findings suggest that nanocapsules embedded in microparticles hold promise for improving the oral bioavailability and efficacy of LPV. By optimizing the formulation, it may be possible to reduce or eliminate the need for ritonavir, minimizing side effects and improving patient compliance. This delivery system, if clinically proven, could revolutionize the way lipophilic PIs are administered, offering new hope for those living with HIV/AIDS.
