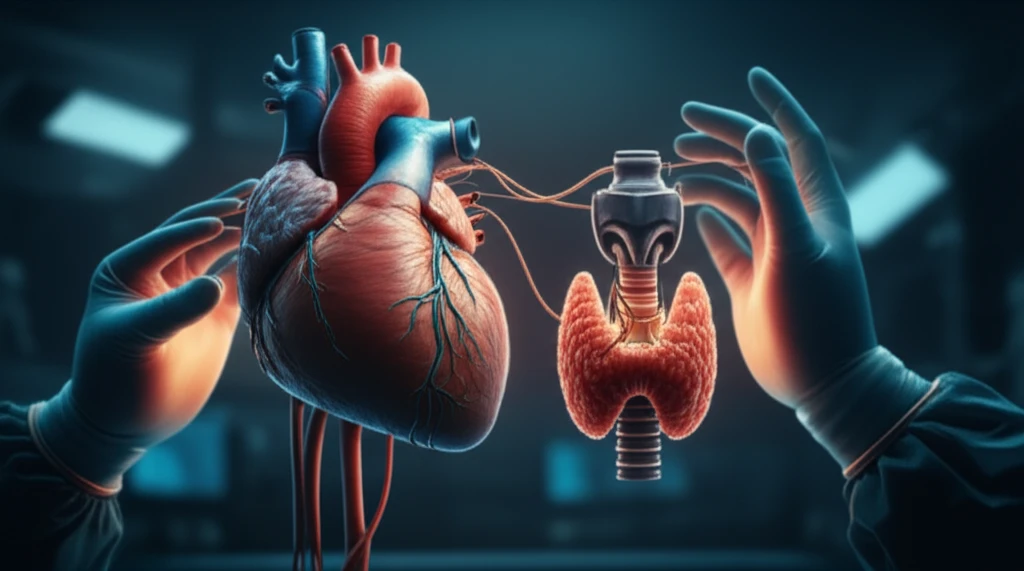
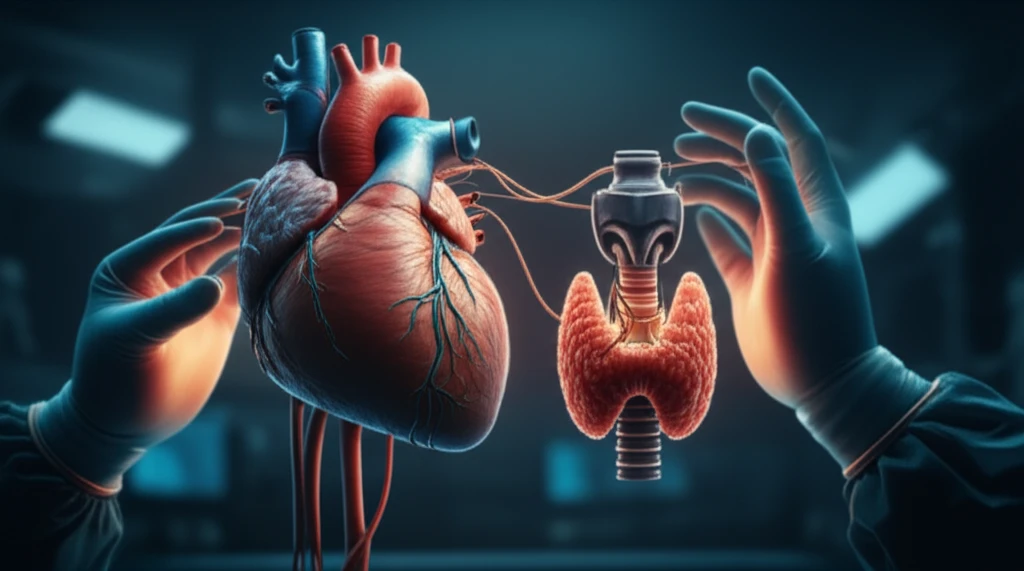
Thyroid Storm on the Table: How to Navigate the Surgical Nightmare of Hypothyroidism During Cardiac Surgery
"Discover how cardiac surgeons manage high-risk hypothyroid patients undergoing coronary bypass, balancing the risks of thyroid correction and surgical intervention."
Managing hypothyroid patients who need coronary artery bypass grafting (CABG) presents a significant challenge for medical teams. These patients often exhibit a depressed cardiac function, showing unpredictable responses to common inotropic drugs, reduced adrenergic responses, impaired baroreceptor reflexes, and increased systemic vascular resistance (SVR). Though successful management strategies have been reported, the inherent risks are undeniably elevated.
When preparing hypothyroid patients for CABG, several critical factors must be considered. These include an increased sensitivity to depressant medications, a hypodynamic cardiovascular system characterized by reduced heart rate (HR) and cardiac output (CO), slowed drug metabolism, impaired ventilatory responses, hypothermia, blunted baroreceptor reflexes, potential primary adrenal insufficiency, and decreased number and sensitivity of β-receptors. Initiating thyroid hormone therapy preoperatively may trigger angina in patients with ischemic heart disease, potentially leading to myocardial infarction, although such occurrences are rare.
This article explores a case of iatrogenic hypothyroidism (induced by radiotherapy) in a patient with unstable angina. The treating physicians hesitated to correct the thyroid status preoperatively due to concerns about provoking a coronary event. This article details how a grossly hypothyroid patient with unstable angina was managed, focusing on the strategies employed to handle both the thyroid imbalance and the cardiac risks.
Case Presentation: Balancing Cardiac and Thyroid Risks
A 58-year-old male with a history of glottic carcinoma, excised five years prior followed by radiotherapy, was scheduled for CABG due to triple vessel disease and unstable angina. Post-radiotherapy, he developed iatrogenic hypothyroidism but was not consistent with his thyroxine medication. Preoperative findings indicated a TSH level of 93 µIU/ml (normal range: 0.45 - 4.5 µIU/ml), Free T3 at 0.02 pg/mL (normal range: 2.3-4.2 pg/mL), and Free T4 at 0.04 ng/L (normal range: 0.8 - 1.8 ng/L).
- Preoperative Management: The patient was maintained on thyroxine 100 µg, isosorbide, atorvastatin, and aspirin.
- Steroid Supplementation: Perioperative steroid supplementation was initiated to mitigate potential adrenal insufficiency associated with hypothyroidism.
- Airway Management: Awake fiberoptic intubation was performed nasally with minimal sedation (fentanyl 100 µg and midazolam 2 mg). Tablet thyroxine 100 µg was administered post-induction via a Ryle’s tube.
Key Takeaways
Based on this experience, it is preferable to optimize a patient’s thyroid status with preoperative thyroxine supplementation, aiming for a near-normal or mildly hypothyroid state, rather than operating on a grossly hypothyroid patient. Levosimendan shows promise as an inotrope to counteract the adverse effects of reduced thyroid hormone levels, particularly in improving cardiac contractility and reducing systemic vascular resistance, especially since it operates independently of β-adrenergic receptors. Further research is needed to fully understand its effectiveness in these critical situations.
