The Silent Killer: Understanding Nontraumatic Diaphragmatic Hernias
"Could that nagging chest pain be something more? Discover the hidden dangers of diaphragmatic hernias and when to seek help."
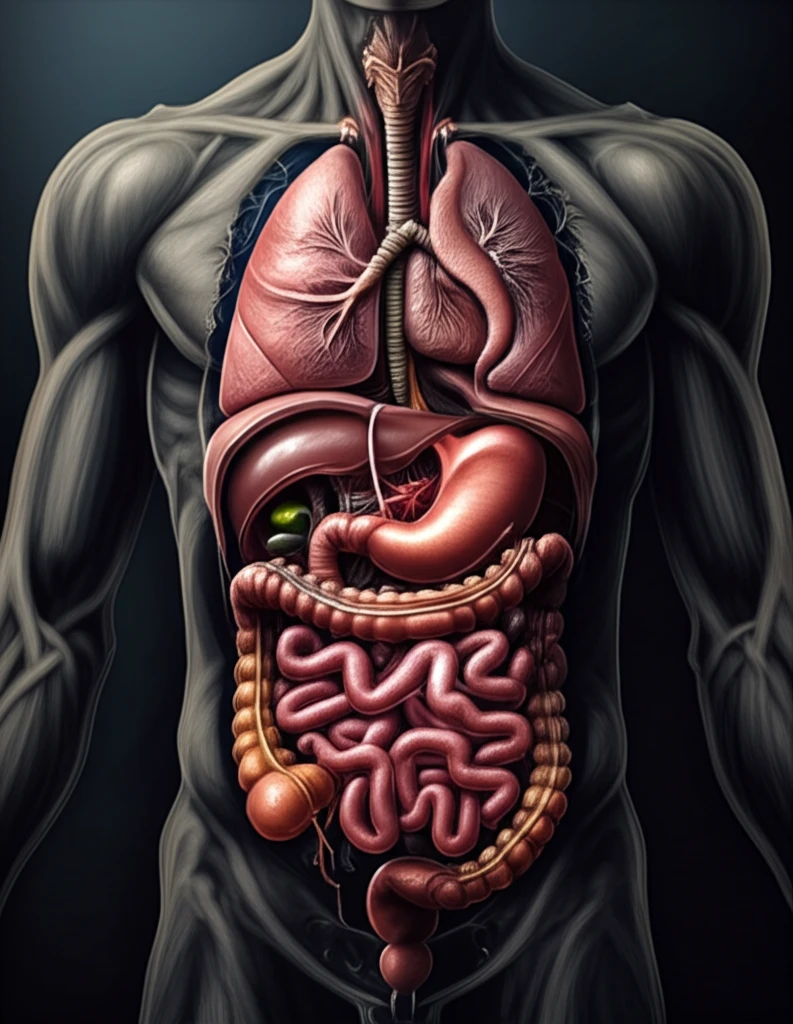
Imagine a scenario where a common complaint like epigastric discomfort turns into a life-threatening emergency. This is precisely what happened in a recent case involving a 43-year-old man with a nontraumatic diaphragmatic hernia, a rare condition where abdominal organs push into the chest cavity through a defect in the diaphragm. While diaphragmatic hernias are often associated with traumatic injuries, this case highlights the critical need to recognize and understand nontraumatic instances, which can present subtly and lead to sudden death.
Diaphragmatic hernias can be broadly classified into two categories: traumatic and congenital. Traumatic hernias result from injuries to the chest or abdomen, while congenital hernias are due to defects present at birth. Bochdalek hernias, the most common type of congenital hernia, occur in the posterolateral region of the diaphragm. Although typically diagnosed in infancy or childhood, these hernias can sometimes go unnoticed until adulthood.
In adults, congenital diaphragmatic hernias are exceedingly rare, with only around 100 symptomatic cases reported in medical literature. What makes these cases particularly challenging is their varied presentation. Unlike infants who often exhibit respiratory distress and cyanosis, adults may experience a range of symptoms, including breathing difficulties, abdominal or chest pain, and even signs of intestinal obstruction. Delayed diagnosis can have dire consequences, making awareness and vigilance essential.
The Case of the Silent Hernia
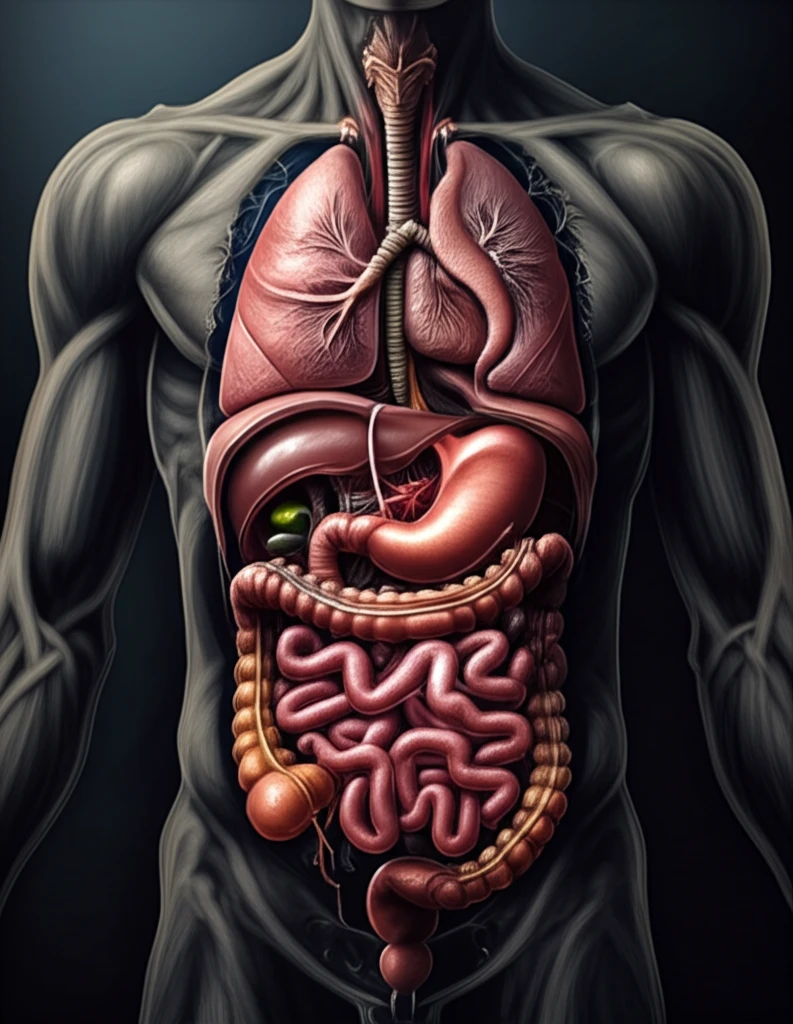
In a recent case, a 43-year-old man with a history of epigastric discomfort and recent respiratory symptoms was found dead at home. He had sought treatment for his discomfort but did not receive further examination. A postmortem CT scan revealed a startling discovery: his stomach had herniated into the left pleural cavity, compressing his left lung and causing a significant shift in the mediastinum, the space between the lungs that houses the heart and major blood vessels.
- A large diaphragmatic defect in the left posterolateral area.
- Herniation of abdominal organs into the left pleural cavity.
- Compression of the left lung and mediastinal shift.
- Marked distention of the stomach with fluid and food residue.
Recognizing the Risks and Seeking Help
While nontraumatic diaphragmatic hernias are rare, this case serves as a critical reminder for both medical professionals and the public. Vague symptoms like persistent epigastric discomfort, chest pain, or unexplained respiratory issues should prompt further investigation. Diagnostic imaging, such as CT scans, can be invaluable in identifying these hernias and preventing potentially fatal outcomes. If you experience any of these symptoms, especially with no known history of trauma, consult your healthcare provider to rule out any underlying conditions. Early diagnosis and intervention can save lives.
